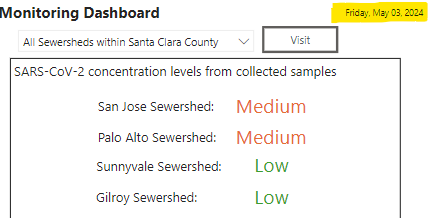
Nationally, we are at “MINIMAL” SARS-CoV-2 virus levels in wastewater, although here in Santa Clara county, Palo Alto and San Jose are still at “MEDIUM” levels of SARS-2 in wastewater as of May 3rd. In the US as a whole, only about 1 in 185 people is infected with COVID now which is a big improvement from the winter.
KP.2 now makes up 24.9% of cases in the United States. KP.1, KP.2 and KP.3 are all JN.1 +FLiRT subvariants. According to data from Yunlong Cao’s lab and from the Sato lab, the Fall 2023 XBB.1.5 booster does not protect well against the JN.1 + FLiRT variants. However, prior JN.1 infection does cause neutralizing antibodies that can fight off the JN.1 + FLiRT variants. This week, the WHO stated that they plan to use JN.1 in the next COVID booster. Some scientists recommend using a JN.1 + FLiRT variant instead for better protection since the next variants will probably descend from those. The FDA will decide on the final Fall 2024 vaccine formula on May 16th.
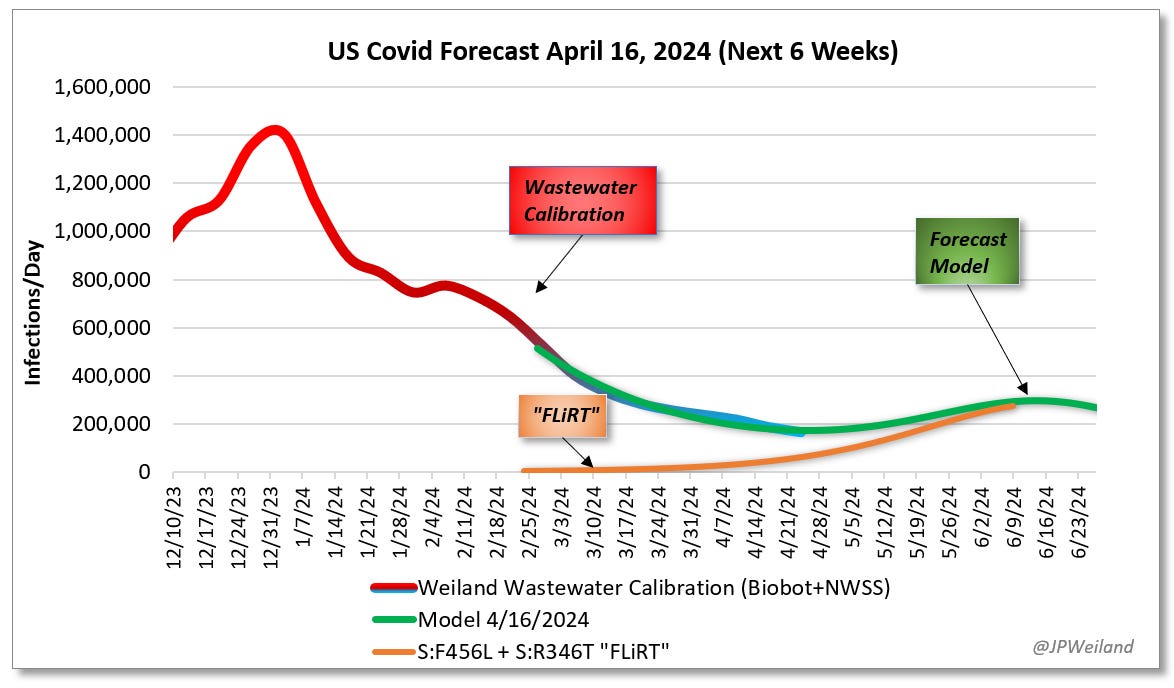
Originally, we were uncertain if the JN.1 + FLiRT variants would cause a new wave of COVID infection or just a wavelet. According to JP Weiland, newer data shows that the FLiRT mutations should cause less of a wave of infection than previously expected which is good news.
Hospitalizations for COVID are the lowest that they have been during the entire pandemic. As of May 1, hospitals are no longer required to report their COVID hospitalization data. But, according to JP Weiland and Katelyn Jetelina, we need hospitalization data in order to better predict upcoming COVID waves. Katelyn Jetelina wrote this week, “[Reporting hospitalization data] is an essential system that will protect the health and safety of our communities.” HHS is accepting comments on this change and you can message them here if you want to request that COVID hospitalization data continue to be posted.
Acute COVID infection
In patients who were hospitalized with severe COVID infection, giving Abatacept, an anti-inflammatory immunomodulating drug used to treat psoriatic arthritis, reduced mortality and improved recovery from acute COVID infection.
Although it is less accurate than PCR testing, a new study shows that it is possible to do viral genomic sequencing of SARS-CoV-2 from home rapid antigen tests. This could be helpful for public health and outbreak surveillance. Potentially, there could be a rapid antigen test exchange program, meaning if you test positive on a rapid home antigen test, you could turn it in so the public health department can do genomic viral sequencing to see if the SARS-CoV-2 virus is getting new mutations. Ideally, the public health department would given you a new rapid home COVID test to replace it.
A new study shows that vaccination protects against acute COVID infection and it also reduces the risk of Long COVID by 25%.
Congratulations to The Sick Times, “the nonprofit newsroom focused on Long Covid and the ongoing Covid-19 pandemic,” who received a $250,000 award from the biotech giving fund Kanro. The award will allow them to expand reporting on Long COVID, acute COVID infections and related chronic diseases.
Societal Costs of Acute COVID infections and Long COVID
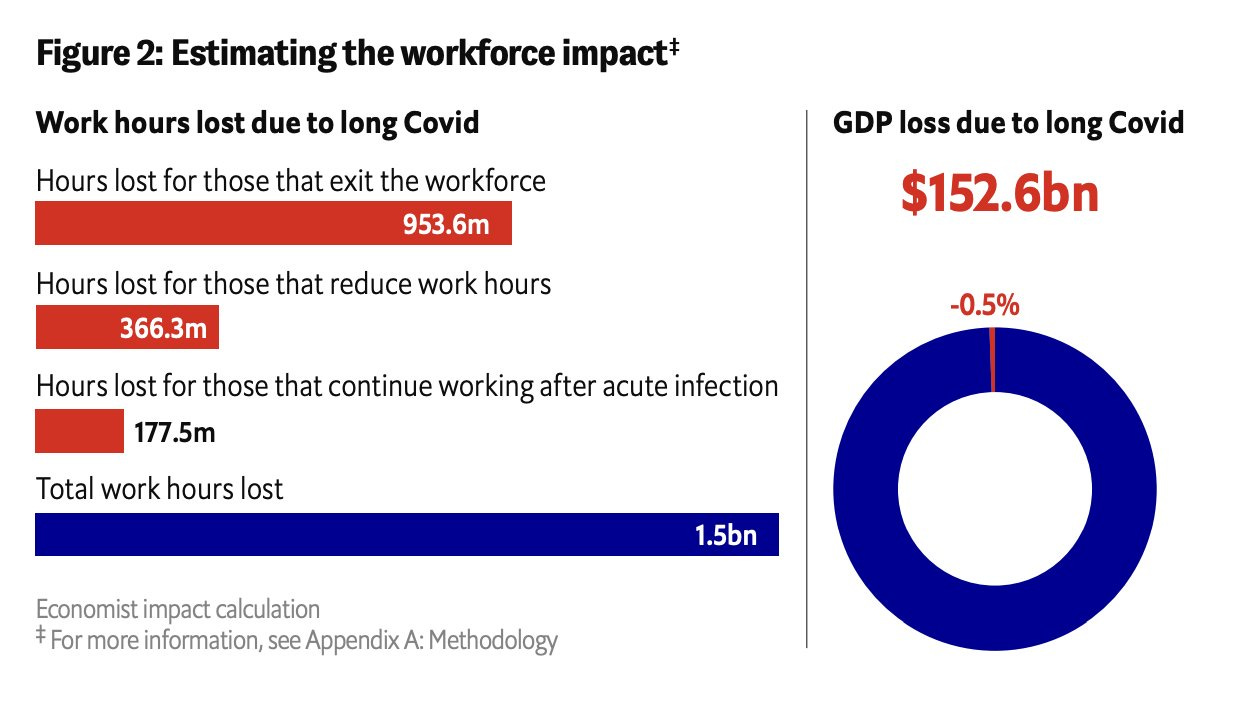
A new report from the Economist shows the enormous economic costs of Long COVID in the US and in other countries because people with Long COVID are no longer able to work. In the United States, Long COVID is estimated to cause a whopping $152.6 Billion GDP loss this year due to lost work hours. In the UK, the equivalent of US$15.5 Billion is expected to be lost in 2024 because of Long COVID disability. The report also reports data on expected economic losses from Long COVID in Brazil, France, Japan, Saudi Arabia and Spain. Preventing COVID infections and Long COVID disability should be a priority for all countries for many reasons.
Studies have shown that acute COVID infections can result in people losing IQ points. As Dr. Ziyad Al-Aly wrote in February, “Generally the average IQ is about 100. An IQ above 130 indicates a highly gifted individual, while an IQ below 70 generally indicates a level of intellectual disability that may require significant societal support… I estimate that a three-point downward shift in IQ would increase the number of U.S. adults with an IQ less than 70 from 4.7 million to 7.5 million – an increase of 2.8 million adults with a level of cognitive impairment that requires significant societal support.” For many reasons, it makes sense for countries to protect their inhabitants from COVID infections.
The UK Office of National Statistics reported that every 1 in 100 children in England and Scotland are suffering from Long COVID. We really need to prevent COVID infections in children and help those who already have Long COVID with support services. Not only could Long COVID be personally and financially devastating to these children and their families, future economic and societal costs could be massive.
Neuro Long COVID
In the last two weeks, there have been several new findings regarding the brain and Long COVID.
When neurofilament light chain (NFL) spills into the blood, it means that there has been damage to axons of nerves in the brain. A new study shows that NFL was found to be elevated in the blood of people with neurologic Long COVID symptoms such as cognitive dysfunction and memory loss. Long COVID is causing brain damage and possible neurodegeneration. These findings add to data from several other studies showing NFL in the blood after COVID infection. A study from 2023 showed elevated NFL in Long COVID. Another study from March 2024 showed elevated neurofilament light chain (NFL) and glial fibrillary acid protein (GFAP) levels 10 months after mild or asymptomatic COVID infections.
A new study of 146,000 people in Norway shows that just having a positive COVID test is associated with an 8-fold increase in memory problems and a 5-fold increase in concentration difficulties at 12 to 18 months after the positive test. We already know that each COVID infection causes us to lose IQ points and this study solidifies those findings. The authors of the Norwegian study concluded, "A positive SARS-CoV-2 test was associated with new onset memory- and concentration problems, anosmia and dysgeusia, dyspnoea and fatigue as well as self-assessed worsening of overall health, which persisted for the length of the follow-up of 22 months, even when correcting for symptoms before COVID-19 and compared to symptoms in negative controls."
A balanced immune response is needed to get rid of invaders such as bacteria while making sure that the immune system does not attack itself like what can happen in autoimmune disease. A new and unexpected discovery shows that there is a body-brain circuit between areas in the brainstem and special nerve tracts within the vagus nerve that control the equilibrium of the immune response in the periphery of the body. Special groups of nerve cells in the vagus nerve go to an area of the brainstem called the caudal Nucleus of the Solitary Tract (cNST) which can turn up or turn down the immune response in the body like a sort of rheostat.
Long COVID and vascular damage to the brain: A group from Harvard used PET scans of the brain to evaluate neuroinflammation in Long COVID. They found that many parts of the brain were affected in Long COVID patients including midcingulate and anterior cingulate cortex, corpus callosum, thalamus, basal ganglia, and at the boundaries of ventricles. Areas of the brain with a thinner blood-brain barrier were most affected. Neuroinflammation seen on PET scan in Long COVID correlated with elevated blood levels of factors related to vascular damage such as fibrinogen.
Figure 2. From https://www.sciencedirect.com/science/article/pii/S0889159124003593#f0005
Viral Persistence and Long COVID
A new article in the Lancet from the Van Weyenbergh lab in Belgium shows that people with Long COVID have a specific SARS-CoV-2 viral RNA signature (high SARS-CoV-2 viral RNA levels and FYN RNA) in their blood that may be used as a biomarker for Long COVID. They also had upregulated ORF1ab RNA in their blood which means that there is ongoing SARS-CoV-2 viral replication. Severe anxiety or depression symptoms in Long COVID were found to be associated with high viral antisense Orf1ab RNA (replicating virus) and low immunometabolism scores as well.
Figure 1 from https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(24)00055-7/fulltext#%20
Another group found that there was viral persistence in solid tissue surgical samples months after mild COVID infection. “Viral RNA was distributed across ten different types of solid tissues, including liver, kidney, stomach, intestine, brain, blood vessel, lung, breast, skin, and thyroid.” Viral persistence in tissues was associated with a 5-fold increase in Long COVID symptoms.
Long COVID and the Gut Microbiome
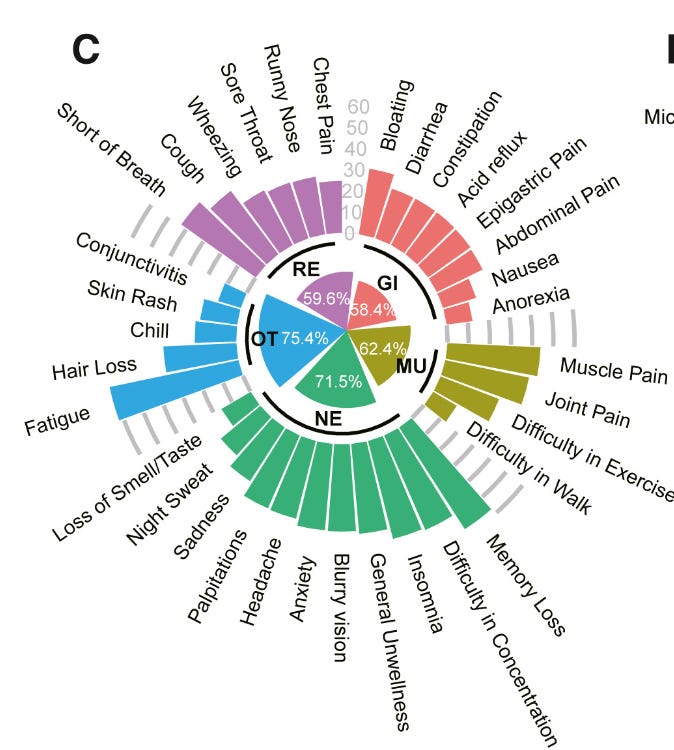
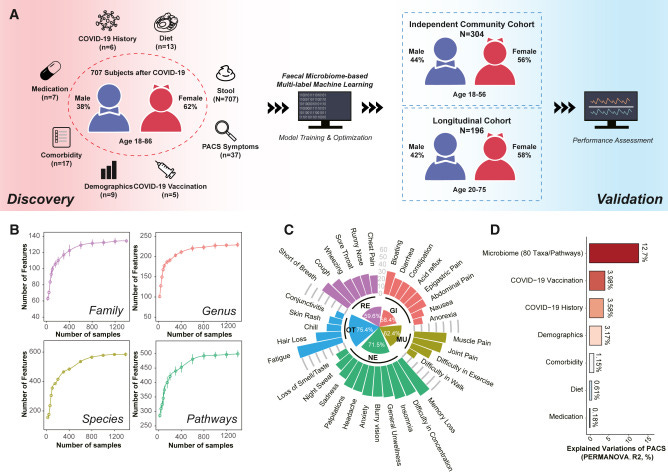
A fascinating article came out this week showing that the particular balance of bacteria in the gut microbiome can predict symptoms in Long COVID. The authors looked at 707 people with post-acute COVID syndrome (PACS or Long COVID) and compared them to two different control groups. They found that analyzing the gut microbiome can also predict who will get Long COVID after acute COVID infection. Overall, Long COVID was associated with low Bifidobacterium adolescentis and Roseburia hominis and increased Clostridium bolteae, Flavonifractor plautii, and urea cycle metabolites. Specific symptoms in Long COVID were related to specific bacteria or metabolites found in the gut microbiome. For instance, anxiety correlated to elevated metabolites from the tricarboxylic acid (TCA) cycle.
Figure 1. The gut microbiome associates with the heterogeneity of post-acute COVID-19 syndrome https://www.sciencedirect.com/science/article/pii/S1931312824001227?via%3Dihub
In non-COVID news, there has been a lot of discussion this week about Avian Influenza A (H5N1) that has been found in dairy cattle across the United States. Migratory wild birds like geese and ducks sometimes carry bird flu. When they fly over a farm, they can contaminate the cattle’s feed with their droppings. It appears that many more cows have been infected than previously thought, as testing of commercial milk showed inactivated pieces of the H5N1 virus in 58 of 150 samples tested in 10 states. Pasteurization kills the H5N1 virus, so it is very important not to drink raw milk. It appears that there has been cow-to-cow transmission of the virus.
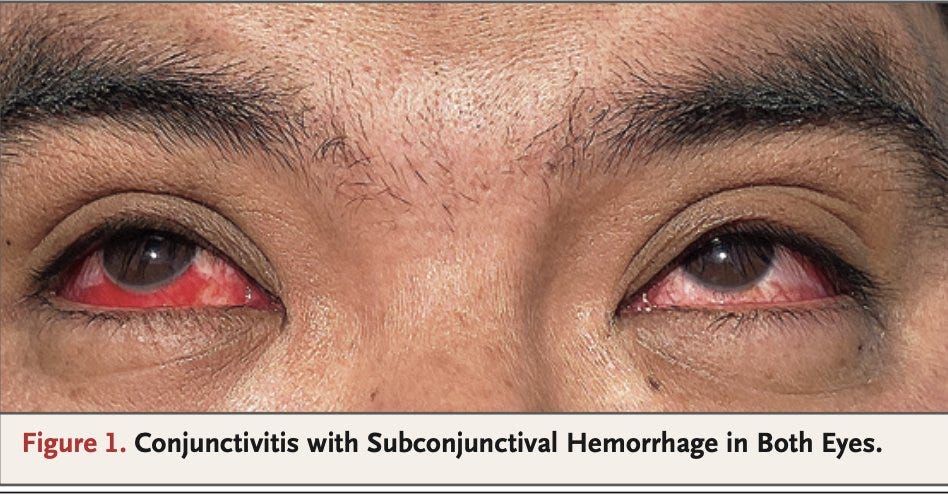
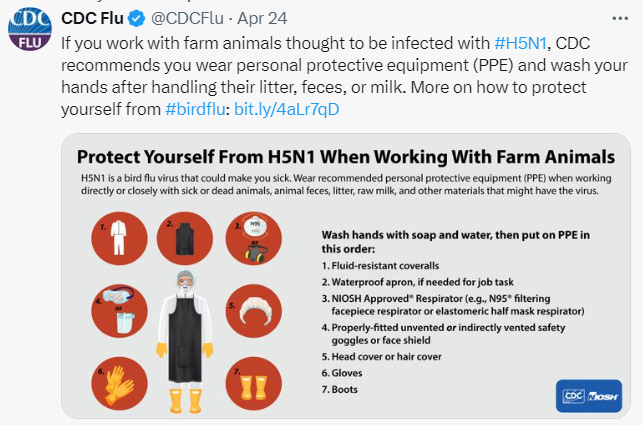
There has also been at least one case of cow-to-human transmission of the H5N1 virus. The infected dairy worker had conjunctivitis with subconjunctival hemorrhage in both eyes (blood-shot eyes), but otherwise had mild symptoms. While it is good for that person that he had mild symptoms, it can be worrisome on a public health level as there may be more people and animals infected that are asymptomatic or very mildly symptomatic. That could allow the virus to spill over to other animal species. In fact, several cats became infected and died after drinking raw cow’s milk on dairy farms. In cats, as in sea lions and in minks, the H5N1 influenza causes systemic illness with a high fatality rate. The CDC now recommends that people who work with farm animals that could be infected with H5N1 should wear PPE including waterproof aprons, N95 masks, goggles, head cover, gloves and boots.
From https://www.nejm.org/doi/full/10.1056/NEJMc2405371
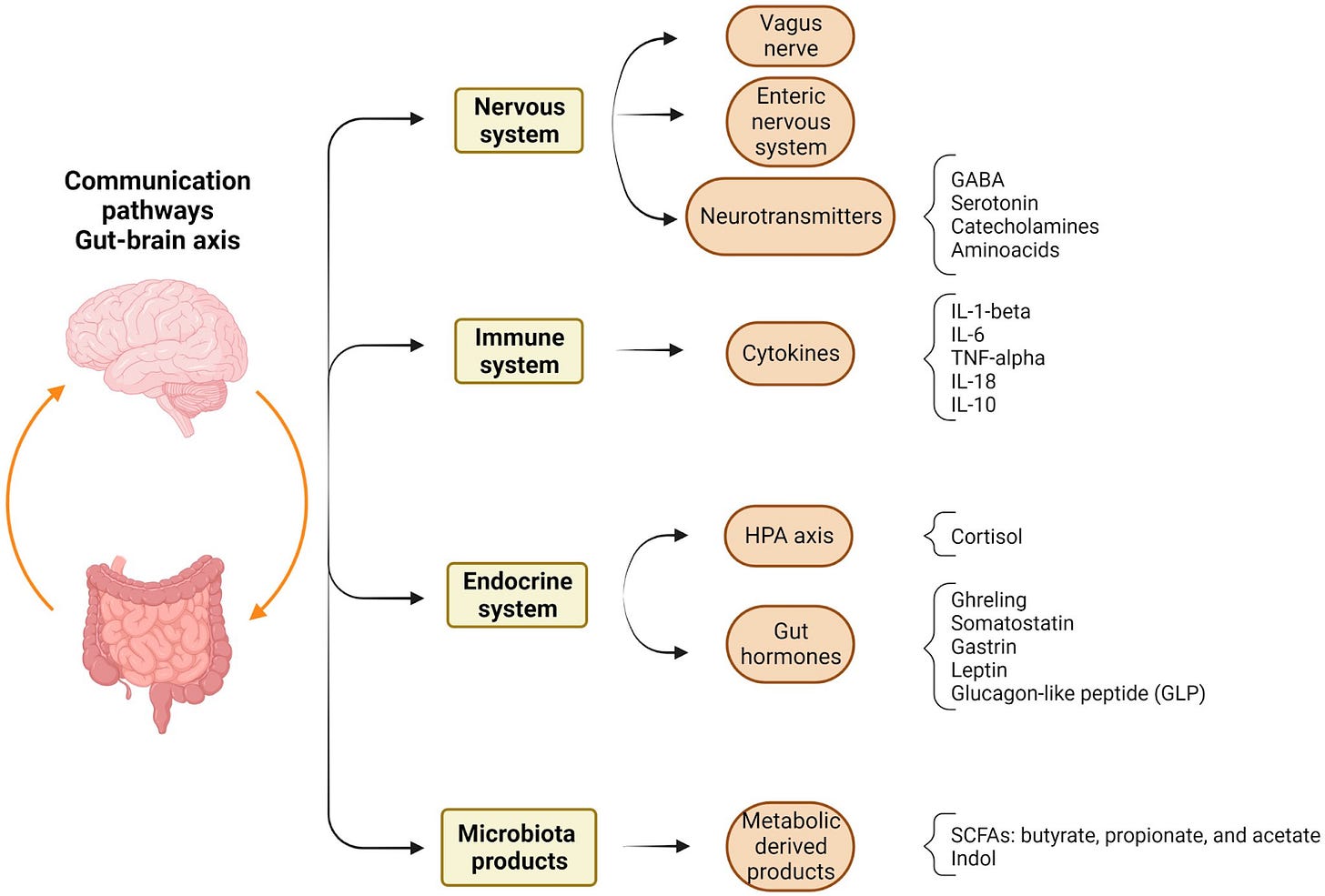
In non-COVID news, Vipin Vashishtha tweeted a great explanatory thread about a new article looking at the gut-brain vagal axis and how it affects memory in the hippocampus of the brain. I find this interesting because the gut-brain-vagus nerve axis may play a role in neuro Long COVID symptoms. In the study, the gut-brain vagal axis was found to affect long-term memories made in the hippocampus of the brain, but not short-term memories. The authors concluded, "our study provides comprehensive insights into the multifaceted involvement of the gut-brain vagal axis in shaping time-dependent hippocampal learning and memory dynamics."
The UnitedHealth Group revealed this week that hackers stole about one third of Americans’ data in a cyberattack of their Change Healthcare unit. In a separate incident, a whistleblower doctor told ProPublica this week that Cigna insurance threatened to fire her for not denying enough patients’ medical requests for care. The CEO of UnitedHealth and the Cigna CEO each made almost $21 Million in salary in 2022. Perhaps some of that money would be better used in paying for patients’ medical care.
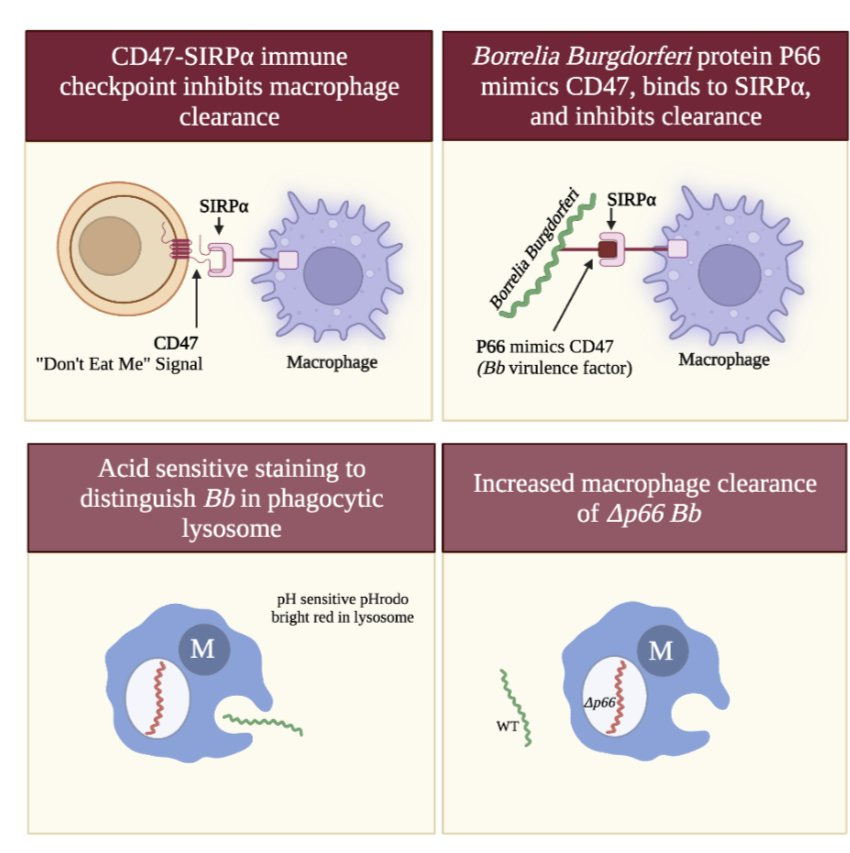
Syphilis typically presents initially with sores or a rash, but more people are showing atypical neurologic symptoms such as headache or hearing or vision problems. A new study shows that Lyme disease bacteria Borrelia burgdorferi hide in plain sight by using their P66 protein to mimic the human CD47 “Don’t eat me” signal. This way, the human immune system does not recognize the bacteria as being foreign.
From https://www.biorxiv.org/content/10.1101/2024.04.29.591704v1
Vitamin D appears to help both mice and humans fight cancer by affecting microbiome-dependent cancer immunity. A new study shows that 10% of people with Multiple Sclerosis may show an MS-specific autoantibody signature years before they become sick. People with sickle cell disease treated with a gene-edited version of their own bone marrow cells that increased levels of fetal hemoglobin were 97% free of sickle cell crises for more than 12 months. The USPSTF is now recommending that women get screening mammograms starting at age 40. ACOG and NCCN have been recommending this for years.
Have a good rest of your weekend,
Ruth Ann Crystal MD
COVID news notes:
US Variant tracker: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
KP.2 is now 24.9% of cases in the United States
Variants around the world: https://outbreak.info/
World wastewater maps (reflects COVID cases): https://www.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082
CDC COVID data tracker: https://covid.cdc.gov/covid-data-tracker/index.html#datatracker-home
CDC COVID Hospitalizations (blue) and Emergency Room (orange) visits tracker: https://covid.cdc.gov/covid-data-tracker/index.html#trends_weeklyhospitaladmissions_7dayeddiagnosed_00
On April 30, they stopped reporting hospitalizations.
US Wastewater Monitoring:
CDC wastewater reporting: https://www.cdc.gov/nwss/rv/COVID19-nationaltrend.html
CDC wastewater map: https://www.cdc.gov/nwss/rv/COVID19-currentlevels.html
Biobot: https://biobot.io/data/
National SARS-CoV-2 data from Sara Anne Willette: https://iowacovid19tracker.org/
Wastewater SCAN: Califostatewide view https://buff.ly/3YObiul
Oakland last reported 4/25/24 Low
Sewer Coronavirus Alert Network (SCAN) project by Stanford University:
Santa Clara County wastewater: https://covid19.sccgov.org/dashboard-wastewater
Marin county: https://coronavirus.marinhhs.org/surveillance
JP Weiland: https://twitter.com/JPWeiland
https://twitter.com/JPWeiland/status/1786544561264664658
May 3rd update:
Infection rates are now near 2023 lows, a month earlier than 2023. If FLiRT only stops the decline, this is a good place to be.
165,000 new infections/day
~2.78 avg total infections per capita across the US
1 in every 201 people currently infected
5/3/24 JP Weiland Forecast: “The model I posted last week suggests a slight uptick from FLiRT, but it's entirely possible that the spring weather is able to subdue the takeover of this more evasive variant. We'll know in a couple of weeks.”
4/26/24 Forecast from JP Weiland:
https://twitter.com/JPWeiland/status/1783991563451777184
Olympics in Paris in July and August 2024
Michael Hoerger modeling: http://pmc19.com/data/,
https://twitter.com/i/lists/1425000060979269635
PMC COVID-19 Forecast, April 29, 2024 (U.S.)
Transmission continues to decline. About 1 in 161 people in the U.S. are infectious, the lowest levels since July 1. Transmission levels are higher than during 27% of the pandemic, but a good time to catch up on delayed care.
4/30/24 Katelyn Jetelina: A Covid-19 update https://buff.ly/3y6KrjD
Today, COVID hospitalization reporting will stop for most hospitals. It will restart October 1st, but starting May 2, you can comment to the HHS asking for hospitalization data to be required again.
JN.1 + FLiRT descendants are expected to cause more of a summer wavelet and not a large wave. Right now, we are at our lowest hospitalizations for COVID since 2020.
"If you’re over 65 and high risk (i.e., in a nursing home, or have comorbidities)," she recommends that you get the Spring COVID booster now.
WHO recommended using JN.1 for the upcoming fall Covid-19 vaccine. The FDA will decide on the Fall vaccine formula on May 16th.
https://twitter.com/JPWeiland/status/1785834535092937214
Comment here to let the HHS know that you want them to continuing to publish COVID hospitalization data https://www.federalregister.gov/documents/2024/05/02/2024-07567/medicare-and-medicaid-programs-and-the-childrens-health-insurance-program-hospital-inpatient
Variants
4/26/24 BioRxiV (Kei Sato lab): Virological characteristics of the SARS-CoV-2 KP.2 variant https://buff.ly/3Wj2opp
https://twitter.com/SystemsVirology/status/1784011459036602700
Summary of Tweet by Kei Sato:
KP.2 = [JN.1 + FLiRT in the spike + V1104L in the spike]
We have seen some of these mutations before.
The FL part of the FLiRT mutations (F456L) was seen in the EG.6 variant.
The RT part of the FLiRT mutations (R346T) was seen in the BQ.1.1 variant.
KP.2 is about 1.2x more transmissible than JN.1.
In pseudovirus testing, KP.2 is less infectious to human cells than JN.1.
KP.2 is more immune evasive to neutralizing antibodies from
The XBB.1.5 vaccine
Prior infection with XBB.1.5, EG.5, HK.3 and JN.1.
These results suggest that KP.2 is one of the most immune-evading variants to date.
KP.2 is more than 3x more resistant to our current 2023-2024 XBB.1.5 booster.
4/22/24 BioRxiV (Y. Cao): Humoral immunogenicity comparison of XBB and JN.1 in human infections https://buff.ly/3w7F6YW
Yunlong Cao and associates looked at breakthrough infections (BTI) of XBB vs. breakthrough infection with JN.1 as a sort of vaccination against the new subvariants of JN.1+ FLiRT mutations. They found that prior JN.1 infection protected against new JN.1 + FLiRT subvariants like KP.2, but prior XBB infection did not.
KP.3 had the most immune evasion.
As Eric Topol tweeted “If you had a JN.1 infection, you're pretty well protected by neutralizing antibodies. But the booster (directed vs XBB.1.5) isn't providing very good protection against FLiRT variants.”
“Results suggest that future SARS-CoV-2 vaccine efforts might benefit from focusing on the JN.1 lineage instead of XBB to better counter current and emerging variants.”
Significant immune evasion of recently emerged JN.1 sublineages, including JN.1+R346T+F456L, with KP.3 showing the most pronounced decrease in neutralization titers by both XBB and JN.1 BTI sera.
WHO recommends that COVID vaccines be updated to a monovalent JN.1 lineage.
4/26/24 WHO: Statement on the antigen composition of COVID-19 vaccines https://buff.ly/4diCaJO
“As the virus is expected to continue to evolve from JN.1, the TAG-CO-VAC advises the use of a monovalent JN.1 lineage as the antigen in future formulations of COVID-19 vaccines.”
Acute COVID infections, General COVID info
4/25/24 JAMA: Abatacept Pharmacokinetics and Exposure Response in Patients Hospitalized With COVID-19 https://buff.ly/4bji545
Abatacept, an anti-inflammatory immunomodulating drug used to treat psoriatic arthritis, reduced mortality and showed better recovery in patients hospitalized with severe COVID-19.
A higher dose than the current abatacept dosing (10 mg/kg intravenously with a maximum of 1000 mg) may be needed for the highest benefit however.
4/12/24 Lancet Microbe (Pardis Sabeti): Optimisation and evaluation of viral genomic sequencing of SARS-CoV-2 rapid diagnostic tests: a laboratory and cohort-based study https://buff.ly/4b8GTfg
Although it is less accurate than PCR testing, this study shows that it is possible to do viral genomic sequencing of SARS-CoV-2 from home rapid antigen tests. This could be helpful for public health and outbreak surveillance.
COVID tests:
https://twitter.com/michaelmina_lab/status/1783221792250732632
Free COVID tests from San Francisco libraries:
Social and Advocacy
Economic costs of Long COVID: https://twitter.com/zalaly/status/1785690574344925193
From Ziyad Al-Aly MD: @zalaly
The economic cost of #LongCovid covid is staggering!
In the US, #LongCovid could result in 1.5 billion work hours lost in 2024 – a potential cost of more than US$152.6 billion
https://impact.economist.com/perspectives/health/incomplete-picture-understanding-burden-long-covid
In the UK, #LongCovid could result in 251.8m work hours lost in 2024 – a potential cost of more than US$15.5bn
The report also includes data on the economic burden of #LongCovid in Brazil, France, Japan, Saudi Arabia and Spain.
Seniors
https://twitter.com/MVGutierrezMD/status/1783561110521511963
Pediatrics
Every 1 in 100 children in England and Scotland now have Long COVID per ONS (Office of National Statistics)
https://twitter.com/jneill/status/1784336169892712672
Vaccines
4/29/24 CIDRAP: COVID booster linked to 25% lower odds of long COVID https://buff.ly/49ZRE2q
"Our findings suggest that ensuring individuals are up-to-date with their COVID-19 vaccinations could be an effective public health strategy for reducing the prevalence of long-COVID,"
4/23/24 JAMA: Serum and Salivary IgG and IgA Response After COVID-19 mRNA Vaccination https://buff.ly/3xRmEUS
In 2021, people who had prior a COVID infection got a large boost of IgA against SARS-2 in their saliva when they received the COVID vaccination. People who were vaccinated against COVID, but had not been infected prior, made much less saliva IgA.
Long COVID
4/20/24 Press release: The Sick Times announces $250,000 in funding to support expanded Long Covid coverage https://buff.ly/4a4v3Sb
“The Sick Times, the nonprofit newsroom focused on Long Covid and the ongoing Covid-19 pandemic, is excited to announce it has received an award of $250,000 from the biotech giving fund Kanro.
“Kanro, along with the Balvi fund — both established by Vitalik Buterin, the co-creator of Ethereum — has supported high-impact research into Long Covid and related chronic diseases by organizations such as the PolyBio Research Foundation and the Patient-Led Research Collaborative.”
7/2024 Brain, Behavior and Immunity (Harvard): Neuroinflammation in post-acute sequelae of COVID-19 (PASC) as assessed by [11C]PBR28 PET correlates with vascular disease measures https://buff.ly/3wjddxc
12 PASC individuals versus 43 normative healthy controls
significantly increased neuroinflammation in PASC versus controls across a wide swath of brain regions including midcingulate and anterior cingulate cortex, corpus callosum, thalamus, basal ganglia, and at the boundaries of ventricles.
PET neuroimaging found neuroinflammation across multiple brain regions in long COVID.
We also collected and analyzed peripheral blood plasma from the PASC individuals and found significant positive correlations between neuroinflammation and several circulating analytes related to vascular dysfunction.
These results suggest that an interaction between neuroinflammation and vascular health may contribute to common symptoms of PASC.
Figure 2:
PolyBio: the is first study to document neuroinflammation in the long COVID brain along with evidence of vascular problems:
5/3/24 PolyBio Research Foundation: LongCOVID brain inflammation associated with vascular problems, Harvard team finds https://buff.ly/4b346ji
“Long COVID brain inflammation is associated with vascular problems, Harvard team finds. Six vascular blood factors including fibrinogen correlated with neuroinflammation in Long COVID.”
Vascular factors included fibrinogen, a protein involved in forming blood clots in the body, and sL-selectin, a molecule that helps immune cells attach to vasculature during inflammation correlated with neuroinflammation in long COVID.
A balanced immune response is needed to get rid of invaders such as bacteria while making sure that the immune system does not attack itself like what can happen in autoimmune disease. Previously unknown that there are areas in the brainstem that get information via the special nerve tracts within the vagus nerve and they control the balance of the immune response in the periphery of the body.
Eric Topol: Our understanding of inflammation and immunity via the body-brain axis jumps forward via discovery of a new circuit (involving cNST, delineated via single-cell sequencing, functional imaging, spatial omics)
5/1/24 Nature (Columbia Univ): A body–brain circuit that regulates body inflammatory responses https://buff.ly/3Qtvn66
Our findings revealed that the Area Postrema (AP) and caudal Nucleus of the Solitary Tract (cNST) in the brainstem were activated in response to stimuli, with minimal activity seen after saline injections.
The AP responds to body malaise while the cNST serves as a vital link in the body-brain connection and is the primary target of the vagus nerve.
If peripheral inflammation is sensed and transmitted by the vagus nerve to the cNST,
“vagal-cNST immune axis”
cNST neurons modulating inflammation
“cNST DBH-expressing neurons receive direct input from the vagal ganglion neurons carrying the anti-inflammatory (expressing TRPA1) and pro-inflammatory (CALCA) signals”
“We propose that the cNST neurons function as a biological rheostat controlling the extent of the peripheral inflammatory response by exerting positive and negative feedback modulation on immune cells. In this regard, we anticipate that the two vagal lines of information, from the periphery to the brain, will interact at the level of the cNST to coordinate the appropriate descending signals. It will be interesting to determine the nature of the cNST DBH+ neurons targeted by each vagal line.
“Dopamine beta-hydroxylase (Dbh) gene as a candidate marker (Fig. 3c). In contrast to previous reports, DBH expressing neurons in the brainstem are almost exclusively located in the cNST.
Explainer article: 5/1/24 Nature: Found: the dial in the brain that controls the immune system https://buff.ly/3Utth7l
Found: the dial in the brain that controls the immune system
Scientists identify the brain cells [in the brainstem] that regulate inflammation, and pinpoint how they keep tabs on the immune response [via input and output from the vagus nerve].
An unexpected finding in the brainstem that could potentially help us to better treat immune dysregulation syndromes like autoimmunity or immune dysregulation from Long COVID.
New article today shows that there are "cells in the brainstem that sense immune cues from the periphery of the body and act as master regulators of the body’s inflammatory response."
"Scientists have known that the brainstem has many functions, such as controlling basic processes such as breathing. However, he adds, the study “shows that there is a whole layer of biology that we haven’t even anticipated”.
two discrete groups of neurons in the vagus nerve: one that responds to pro-inflammatory immune molecules and another that responds to anti-inflammatory molecules. These neurons relay their signals to the brain, allowing it to monitor the immune response as it unfolds.
5/1/24 MedRxiV: Temporal trajectories of COVID-19 symptoms in adults with 22 months follow-up in a prospective cohort study in Norway. https://buff.ly/3JHqa77
Cognitive and physical symptoms before, during, and after a positive- or negative SARS-CoV-2 test and in untested controls.
A prospective cohort study. Setting Norway, March 2020 to July 2022
N =146,065 volunteers. (15,737 participants had a positive SARS-CoV-2 test, 67,305 a negative test, and 37,563 were still untested)
A positive SARS-CoV-2-test was associated with the following persistent symptoms, compared with participants with a negative test:
Memory problems (3 to 6 months after a positive test: odds ratio (OR) 9.1)
Memory problems (12 to 18 months: OR 7.8),
Concentration problems (3 to 6 months: OR 6.1)
Concentration problems (12 to 18 months: OR 5.3),
anosmia and dysgeusia, dyspnoea and fatigue and self-assessed worsening of overall health.
"A positive SARS-CoV-2 test was associated with new onset memory- and concentration problems, anosmia and dysgeusia, dyspnoea and fatigue as well as self-assessed worsening of overall health, which persisted for the length of the follow-up of 22 months, even when correcting for symptoms before COVID-19 and compared to symptoms in negative controls."
4/27/24 Nature Molecular Psychiatry (Brasil): Long COVID: plasma levels of neurofilament light chain (pNfL) in mild COVID-19 patients with neurocognitive symptoms https://buff.ly/4de8IEF
n = 63 people with Long COVID underwent neurocognitive testing.
Higher pNfL levels in plasma correlated with cognitive impairment and severe fatigue in Long COVID patients.
pNfL levels are significantly higher in long COVID patients with mild acute COVID-19 and neurocognitive symptoms when compared to HC.
Additionally, poorer cognitive performance and worse fatigue status correlated with higher pNfL levels.
These results demonstrate the potential of pNfL as a biomarker of the CNS ongoing injury in long COVID patients with cognitive impairment and fatigue.
This can contribute to a better understanding of the mechanism of long COVID and to identify who will need continuous monitoring and treatment support. Further studies are needed to elucidate the extension of the CNS damage and possible neurodegenerating consequences.
Fig. 1: Comparison of pNfL levels between HC samples collected before the pandemic and long COVID patients with alteration of at least one neurocognitive test.
Fig. 3: Comparison of pNfL levels (pg/mL) between long COVID patients with cognitive impairment and fatigue, and long COVID patients without cognitive impairment and fatigue.
4/8/24 Dani Beckman PhD:
https://twitter.com/DaniBeckman/status/1777248177877573952
“Biomarkers for neuronal damage after Covid infection: even mild or asymptomatic #SARSCoV2 infection leads to reflections of neuron (Nfl marker) and astrocyte (Gfap marker) breakdown in the blood up to 10 months after the resolution of the infection.
“Nfl is a protein only found in neurons. So, if it appears in your blood, you can imagine what it means.
“Now image all these people getting #COVID several times per year.
Protect your neurons, people! Adult neurogenesis in the human brain is not substantial; you are born with all the neurons you have, so you better take good care of them.”
3/18/24 Nature: Neurofilament light chain and glial fibrillary acid protein levels are elevated in post-mild COVID-19 or asymptomatic SARS-CoV-2 cases https://buff.ly/3PWlSMy
Cognitive function and blood tests were performed on 147 people with mild or asymptomatic COVID infection compared to 82 healthy controls (HC) without COVID infection.
Ten months after resolution of mild or even asymptomatic SARS-CoV-2 infection, some people still had abnormal blood levels of NFL and/or GFAP meaning that they had ongoing damage to their brains.
Neurofilament light chain in the serum (sNfL) means that there is ongoing damage to the axons of nerves in the brain (or spinal cord). Glial fibrillary acidic protein (sGFAP) in the blood means that there is abnormal activation of astrocytes in the brain.
4/7/24
https://twitter.com/DaniBeckman/status/1777121079104077997
@DaniBeckman PhD: Neuroscientist specialized in high-resolution microscopy at the California National Primate Center.
Biomarkers for #LongCovid
The table below summarizes biomarkers that can potentially indicate differences in long Covid patients and, to some extent, other post-viral illnesses.
All these protein targets can be measured in blood or spinal fluid using commercially available assays, but we know this does not imply patients will have access to them. However, I think it is a good list for patients and M.D.s to discuss together.
I would love to hear from neuro LC patients and neurologists if anyone has experience with measuring GFAP and NFL. Is it two of the proteins I am constantly showing as altered with brain microscopy after the covid infection.
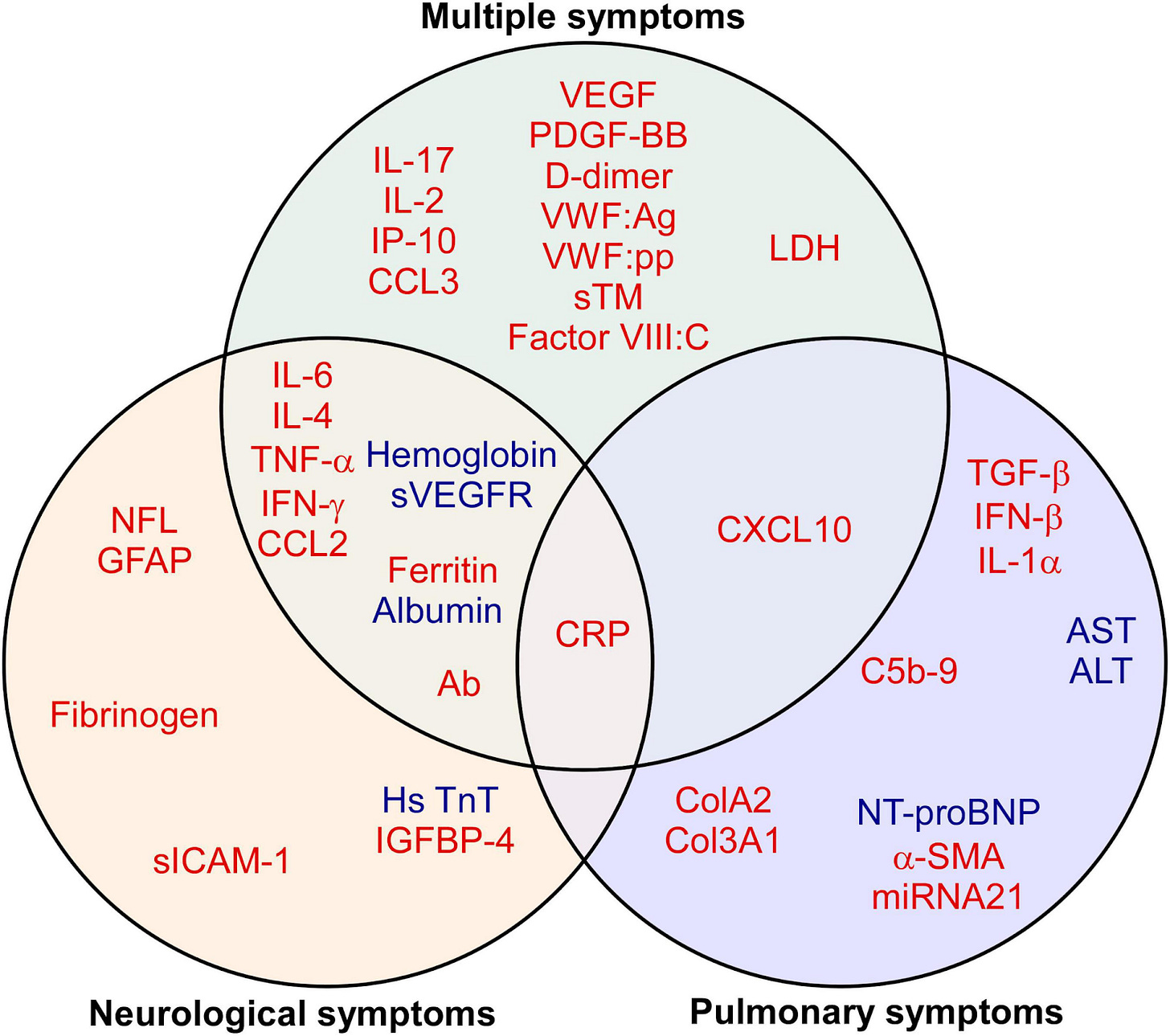
1/20/2023 Frontiers in Medicine, Review: Biomarkers in long COVID-19: A systematic review https://buff.ly/43QrxJH
Long COVID biomarkers: increased IL-6, CRP, TNF-alpha
Neuro Long COVID: high neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP)
Pulm symptoms in LC: high TGF-beta
“the up-regulated levels of neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP) in serum may indicate neuronal damage in the progression of neurodegenerative diseases, such as Alzheimer’s disease (10) or Parkinson’s disease (11).”
Figure 3. Biomarkers Red indicates up-regulated, while blue refers to down-regulated biomarkers.
Figure 4. Biomarkers of long COVID symptoms.
Red indicates up-regulated, while blue refers to down-regulated biomarkers.
Supplementary: PubMed search terms used for this article https://www.frontiersin.org/articles/10.3389/fmed.2023.1085988/full#supplementary-material
—
Van Weyenbergh lab study
4/26/24
https://twitter.com/EricTopol/status/1783877311324205477
4/24/24 Lancet Microbe (Van Weyenbergh lab): Blood transcriptomic analyses reveal persistent SARS-CoV-2 RNA and candidate biomarkers in post-COVID-19 condition https://buff.ly/3Uz7LPS
N = 48 Long COVID and N=12 recovered controls
SARS-CoV-2 viral RNAs were upregulated, except for the spike protein RNA so this is not related to vaccination.
Viral persistence: High SARS-CoV-2 viral RNA levels and FYN RNA levels in the blood predict Long COVID (with AUC .94). It is best to test them together.
The upregulation of antisense ORF1ab RNA suggests ongoing viral replication.
Multivariable logistic regression identified antisense SARS-CoV-2 and FYN RNA concentrations as independent predictors of Long COVID.
Severe anxiety or depression symptoms in Long COVID were found to be associated with high viral antisense Orf1ab RNA and low immunometabolism scores.
4/26/24 Johan Van Weyenbergh Tweet thread
https://twitter.com/johanvawe/status/1783825920337551405
What did we find?
1. viral RNAs were higher in #LongCovid: Nucleocapsid, ORF7a, ORF3a, Mpro (=Paxlovid target), and antisense ORF1ab RNA. Of note, presence of antisense RNA suggests ongoing viral replication
2. #SARSCoV2-related host RNAs ACE2/TMPRSS2, DPP4/FURIN also higher!
Looking at viral RNAs above cutoff (red line below) comparing patients and controls: antisense (65% vs 25%), ORF7a (60% vs 25%), Nucleocapsid (50% vs 8%), total blood viral load (60% vs 8%). Remarkably, Spike RNA was low in all cases =infection not vaccine-derived
3. Looking at the immune response in #LongCovid:
memory B-cell genes up (in green below) include IgE (resonates with new onset allergies in patients) and platelets genes up (salmon colored) -> hypercoagulative state @resiapretorius or viral reservoir =Bomsel lab @UParisDescarte
Immune status in #LongCovid is neither hyperinflammation nor immunodepression BUT we find lower lymphocyte activation (yellow dots) and lower #immunometabolism (blue dots) =similar to findings @RobWust team (but we find lower IDO1 not higher IDO2).
Long COVID and the Gut Microbiome
4/23/24 Cell Host & Microbe (Hong Kong): The gut microbiome associates with phenotypic manifestations of post-acute COVID-19 syndrome (PACS or Long COVID) https://buff.ly/4ddc2Qg
"Gut microbiome-based multi-label machine learning accurately predicts upcoming long-term symptoms after acute COVID19."
n = 707 with PACS, who were on average 5 months post-COVID-19 (Figure 1C),
post-COVID subjects without PACS (n = 201) and a cohort of healthy subjects without COVID-19 exposure (n = 653) were employed as non-PACS controls.
The most common symptoms of PACS were fatigue (62.1%), memory loss (57.1%), difficulty in concentration (48.7%), and insomnia (47.7%).
These symptoms were further classified into five categories, including GI, RE, musculoskeletal (MU), neurological (NE), and other (OT).
Collectively, 73.3% of the subjects reported two or more symptoms, with a median of eight symptoms.
Fecal-microbiome-based multi-label machine learning model to predict the multiple symptoms of PACS.
The top-ranked gut microbiome features for PACS include:
depletion of Bifidobacterium adolescentis and Roseburia hominis, pyruvate fermentation to acetate and lactate II, and
enrichment of Clostridium bolteae, Flavonifractor plautii, and the urea cycle.
gut dysbiosis may play a role in the pathogenesis of PACS.
No difference was found in PACS-related host factors (alcohol, BMI, gender, COVID-19 vaccine, and suspected SARS-CoV-2 variants) and dietary patterns among enterotypes, suggesting that the difference in microbiome was not driven by these confounders (Figure 2C).
Figure 1. The gut microbiome associates with the heterogeneity of post-acute COVID-19 syndrome
Microbiome predicted Long COVID (PACS) subtypes: GI, gastrointestinal; RE, respiratory; MU, musculoskeletal; NE, neurological; OT, other.
Fig 1C: Microbiome predicted Long COVID (PACS) subtypes: GI, gastrointestinal; RE, respiratory; MU, musculoskeletal; NE, neurological; OT, other.
Figure S1. Alteration of gut microbiome in subjects with PACS. Related to Figure 2.
(D) Associations between gut microbiome composition and function among the three cohorts assessed by MaAsLin2 (FDR<0.05).
The gut microbiome explains a large part of heterogeneity in PACS.
Several common biomarkers for PACS, including potential probiotics such as Bifidobacterium adolescentis, Roseburia hominis, and the bacterial pathways producing short-chain fatty acids (SCFAs).
Moreover, we also observed the enrichment of opportunistic pathogens, such as Klebsiella quasipneumoniae (bad) and Ruminococcus gnavus (bad), in subjects with PACS. Both have been associated with multiple human diseases.
Our analysis showed that the pathway of the tricarboxylic acid (TCA) cycle exhibited a positive association with anxiety specifically. Biomarker.
4/25/24 JAMA: Psychiatric Symptoms and Care Access Among Adults With Post–COVID-19 Condition https://buff.ly/4aSSTBI
n = 25,122 people with Long COVID
People with Long COVID were approximately twice as likely to report depression and anxiety symptoms than other US adults, but they often had cost-related barriers to getting therapy.
After mild COVID infection, detection of viral RNA in multiple solid tissues surgical samples months later was associated with a 5-fold increase in Long COVID symptoms.
4/22/24 Lancet Infectious Disease: The persistence of SARS-CoV-2 in tissues and its association with Long COVID symptoms: a cross-sectional cohort study in China https://buff.ly/49VpFkd
Residual SARS-CoV-2 can persist in patients who have recovered from mild COVID-19 and that there is a significant association between viral persistence and long COVID symptoms.
Mild COVID infections of Omicron in Dec 2022.
Solid tissue samples including liver, kidney, stomach, intestine, brain, blood vessel, lung, breast, skin, and thyroid:
At 1 month, 30% had viral RNA persistence
At 2 months, 27% had viral RNA persistence
At 4 months 11% had viral RNA persistence
Additionally, 43% had subgenomic RNA as well as viral RNA.
Detection of viral RNA in recovered patients was significantly associated with the development of long COVID symptoms (odds ratio 5·17, 95% CI 2·64–10·13, p<0·0001).
Patients with higher virus copy numbers had a higher likelihood of developing long COVID symptoms.
3/2024 CRIO Conference
Poster from Morgane Bomsel’s lab in Paris
Persistence of SARS-CoV-2 in platelets and megakaryocytes in Post-acute Sequelae of SARS-CoV-2 (Long COVID) https://www.croiconference.org/wp-content/uploads/sites/2/posters/2024/347.pdf
Megakaryocyte (MK) frequency is increased in Long COVID
Megakaryocytes contain SARS-CoV-2 Spike and dsRNA in long COVID. Megakaryocytes are the precursors to platelets. When infected, they release platelets that contain SARS-CoV-2 Spike and RNA in Long COVID.
Platelets are important for hemostasis and clotting, but they also carry 5-HT (Serotonin). Peripheral serotonin is low in Long COVID. Disruption of Serotonin can cause problems with emotions, sleep, anxiety and depression.
SARS-2 spike protein can be found in some people with Long COVID.
“Conclusions: In Long COVID, SARS-CoV-2 persists and replicates in MKs that in turn produce platelets containing virus. Circulating spike might be an additional sign of viral persistence that could serve as a Long COVID biomarker. The persistence of the virus could lead to abnormal platelet activation and formation of microclots, contributing to the various symptoms observed in LongCOVID and to deregulation of serotonin uptake, favoring neurocognitive symptoms found in longCOVID.”
https://twitter.com/thephysicsgirl/status/1783893892573942161
Ibudilast info from MS Canada https://mscanada.ca/ibudilast
Overview:
AKA MS-166 from MedicNova given as 100mg/day.
Phosphodiesterase inhibitor; neuroprotective
Emerging Treatment for Primary Progressive MS (PPMS) and secondary progressive MS (SPMS)
Ibudilast works by suppressing three cell signaling molecules that promote inflammation: IL-1β, TNF-α, and IL-6. Ibudilast may also upregulate anti-inflammatory cell signaling molecules resulting in neuroprotective effects and reduced neuroinflammation. Ibudilast has been approved in Japan and Korea to treat asthma and cerebrovascular disorder for over 20 years.
Phase II Trial- Relapsing-Remitting MS (RRMS)
Treatment with ibudilast had no effect of the treatment on the number of active lesions or relapse rate. There may be a neuroprotective effect as fewer people witnessed confirmed disease progression and displayed reduced brain atrophy.
4/29/24 Press Release: BioVie Awarded up to $13.1 Million in Funding from U.S. Department of Defense to Evaluate Bezisterim (NE3107) for the Treatment of Long COVID https://buff.ly/4aWpeHZ
Plans a Phase 2b clinical trial of Bezisterim, an oral anti-inflammatory and insulin-sensitizer that permeates the blood brain barrier.
5/3/24
https://twitter.com/dysclinic/status/1786542607746675180
Presentation of Long COVID with facial and extremity numbness
POTS and Autoimmunity, a review
4/20/24 J of Personalized Medicine: Autoimmunity in Syndromes of Orthostatic Intolerance: An Updated Review https://buff.ly/4bcxymJ
RAC: Could PEG-lambda interferon be helpful in Long COVID?
2/9/2023 Stanford Medicine: Single drug injection wards off COVID-19 hospitalizations, in Stanford Medicine-led trial https://buff.ly/4bd98t9
In an international (Brasil, Canada), multicenter, pivotal Phase 3 trial, a single under-the-skin injection of pegylated lambda-interferon, or PEG-lambda, decreased hospitalizations by half with low side effects.
Jeffrey Glenn, MD, PhD, Stanford professor of medicine and of microbiology and immunology and director of ViRx@Stanford, a Stanford Medicine program devoted to discovering and developing novel antiviral agents to prepare for pandemics.
2/8/2023 NEJM: Early Treatment with Pegylated Interferon Lambda for Covid-19 https://buff.ly/3lrFtYN
Among predominantly vaccinated outpatients with Covid-19, the incidence of hospitalization or an emergency department visit (observation for >6 hours) was significantly lower among those who received a single dose of pegylated interferon lambda than among those who received placebo.
His idea: Dating app to meet other people with ME/CFS for friendship using Hinge app and Skarsvag, Norway.
https://twitter.com/RorPreston/status/1784226449844478192
AI:
https://twitter.com/EricTopol/status/1784936718283805124
4/29/24 Nature: AI-enabled electrocardiography alert intervention and all-cause mortality: a pragmatic randomized clinical trial https://www.nature.com/articles/s41591-024-02961-4
Randomized trial shows that AI reduced mortality 31% (absolute 7 per 100 patients) in “pre-specified high-risk group”
Med-Gemini
https://twitter.com/alan_karthi/status/1785117444383588823
“Delighted to share Med-Gemini - our new family of multimodal models for medicine unlocking new possibilities for health - https://arxiv.org/pdf/2404.18416”
3/28/24 NEJM AI: Disorder-Free Data Are All You Need — Inverse Supervised Learning for Broad-Spectrum Head Disorder Detection https://buff.ly/3JCQzTn
Our novel AI-based system utilizing ISL can accurately and broadly detect disorders without requiring disorder-containing data. This system not only outperforms previous AI-based systems in terms of disorder detection but also provides visually understandable clues, enhancing its clinical utility.
4/27/24
https://twitter.com/glfceo/status/1784226184764731729
Other news:
Vagus nerve: Gut-Brain Vagal Axis and Hippocampal memory
Great tweet thread by Vipin M. Vashishtha on article
https://twitter.com/vipintukur/status/1785520823454900664
Figure from: Vipin M. Vashishtha
Until now, linking the vagus nerve to the hippocampus & its contribution to learning & memory dynamics remain still elusive.
4/30/24 BioRxiV: The gut-brain vagal axis scales hippocampal memory processes and plasticity https://buff.ly/4dp7MNK
"In conclusion, our study provides comprehensive insights into the multifaceted involvement of the gut-brain vagal axis in shaping time-dependent hippocampal learning and memory dynamics."
Vipin: “The results indicate that the integrity of the vagal axis is essential for long-term recognition memories, while sparing other forms of memory.”
“The study provides comprehensive insights into the multifaceted involvement of the gut-brain vagal axis in shaping time-dependent hippocampal learning and memory dynamics.”
5/1/24 Reuters: UnitedHealth says hackers potentially stole a third of Americans' data https://buff.ly/44oNXSG
Cyberattack on the company's Change Healthcare unit, which processes around 50% of all medical claims in the U.S. a third" of Americans' protected health information and personally identifiable information was stolen.
"UnitedHealth Group has not revealed how many patients' private medical records were stolen, how many providers went without reimbursement, and how many seniors are unable to pick up their prescriptions as a result of the hack," said Wyden.
5/1/24 STAT News: With younger women getting breast cancer, national panel lowers mammogram screening age to 40 https://buff.ly/3Qs4uzp
USPSTF recommends mammograms starting at age 40 which is what ACOG and NCCN have been recommending for years.
Black women are more likely to get breast cancer at younger ages and be diagnosed with more aggressive tumors. Lowering the age of screening will hopefully help narrow health disparities as well.
4/20/24 BioRxiV (Michal Tal et al.): P66 is a bacterial mimic of CD47 that binds the anti-phagocytic receptor SIRPα and facilitates macrophage evasion by Borrelia burgdorferi https://buff.ly/3UkznXW
"Lyme bacteria mimic our own “don’t eat me” signal with their P66 protein to hide in plain sight!!! This tricks our SIRPa protein to trigger the breaks on immune clearance!" - Michal Tal on Twitter
4/29/24 ProPublica: A Doctor at Cigna Said Her Bosses Pressured Her to Review Patients’ Cases Too Quickly. Cigna Threatened to Fire Her. https://t.co/noy1grsMYN
“Deny, deny, deny. That’s how you hit your numbers,” Day said.
4/29/24 HealthDay: Syphilis Is Increasingly Displaying Atypical, Severe Symptoms https://buff.ly/3WlOkLP
Syphilis usually presents with sores or a rash, but there's a rise in cases without these symptoms.Instead, people are coming to doctors with headache, hearing or vision issues.
"neurologic, ocular, and otic (NOO)" -- affecting the brain, eyes and/or hearing -- forms of syphilis, which can often be severe.
Newborn syphilis rates have increased significantly as well.
4/25/24 Science: Vitamin D regulates microbiome-dependent cancer immunity https://buff.ly/3xX4FMU
Vitamin D supplementation in mice affects gut bacteria and the microbiome and improves cancer immunotherapy and antitumor immunity.
In humans, low vitamin D levels were correlated with tumor development, and gene signatures of vitamin D activity were associated with improved patient responses to immunotherapy.
4/24/24 NEJM: Exagamglogene Autotemcel for Severe Sickle Cell Disease https://buff.ly/3xTmNr3
30 patients with severe Sickle Cell Disease who were treated with gene-edited autologous hematopoietic stem and progenitor cells (exa-cel to increase fetal hemoglobin), 97% were free from vaso-occlusive crises 12 months or more.
Avian Flu H5N1
CDC recommends farm workers wear PPE
https://www.cdc.gov/flu/pdf/avianflu/protect-yourself-h5n1.pdf
5/1/24 (7/2024 Early Release) from the CDC: Highly Pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b Virus Infection in Domestic Dairy Cattle and Cats, United States, 2024 https://buff.ly/3y0DCjQ
Cows with H5N1 eat less and have a drop in milk production, but cats who drank the raw milk died from systemic H5N1 flu.
There was abundant virus shedding found in milk.
Cow-to-cow transmission appears to have occurred.
"Highly pathogenic avian influenza (HPAI) viruses pose a threat to wild birds and poultry globally, and HPAI H5N1 viruses are of even greater concern because of their frequent spillover into mammals."
Minks and sea lions have had large die offs from H5N1.
"In conclusion, we showed that dairy cattle are susceptible to infection with HPAI H5N1 virus and can shed virus in milk and, therefore, might potentially transmit infection to other mammals via unpasteurized milk. A reduction in milk production and vague systemic illness were the most commonly reported clinical signs in affected cows, but neurologic signs including blindness and death rapidly developed in affected domestic cats."
5/3/24 NEJM: Highly Pathogenic Avian Influenza A(H5N1) Virus Infection in a Dairy Farm Worker https://buff.ly/3wbp28G
The first documented case of human H5N1 Avian Flu of a dairy worker in Texas.
With mild symptoms in humans there may be other humans who have been infected as well.
4/24/24 Eric Topol MD: A Bird Flu H5N1 Status Report https://buff.ly/3JyUBMI
Clear reporting of the latest on H5N1 in cattle and poultry.
Viral remnants seen in commercial milk, but pasteurization killed the virus.
Multiple Sclerosis:
4/20/24 Bloomberg: This Multiple Sclerosis Breakthrough Could Be A Breakthrough https://buff.ly/3vUvT6l
A UCSF team has identified a unique immune signature in 10% of patients with MS that appears years before their symptoms.
4/19/24 Nature: An autoantibody signature predictive for multiple sclerosis https://buff.ly/3UaaGxg
Autoantibody reactivity was found years before developing MS symptoms and was associated with higher levels of serum neurofilament light (sNfL) which is a marker of axonal injury.
“In this study, an MS-specific autoantibody signature was identified in a subset of patients years before their first clinical MS attack. This same signature was validated using two different methods in an independent, prospective cohort of patient samples.”

















































Thank you so very much. Hope you had a refreshing vacation!