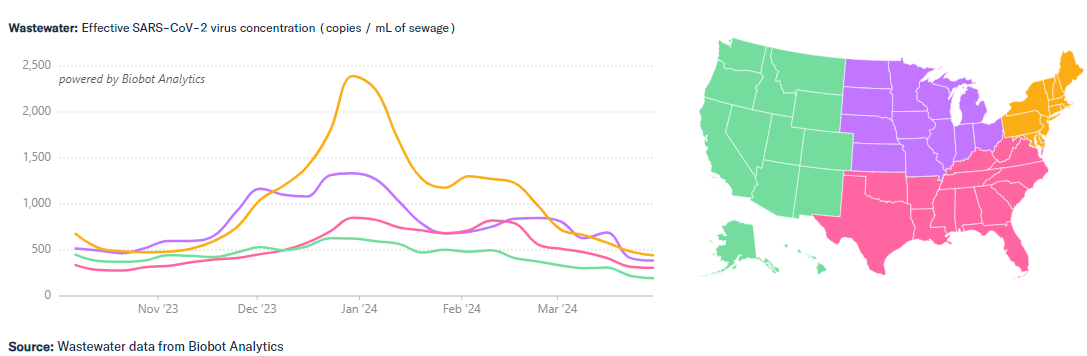
Regarding COVID, we are in a good place for now. Wastewater virus levels are “LOW” in general for the nation, although SARS-CoV-2 wastewater levels are “VERY HIGH” in New Mexico and are “HIGH” in Missouri. Hospitalizations, Emergency Department visits and deaths from COVID continue to decrease significantly. According to JP Weiland, there are about 245,000 new COVID infections each day in the United States, with 1 in every 135 people currently infected. This is a huge improvement from the end of December 2023 when there were about 1.4 million new cases each day.
From: https://twitter.com/JPWeiland/status/1776381105353969994
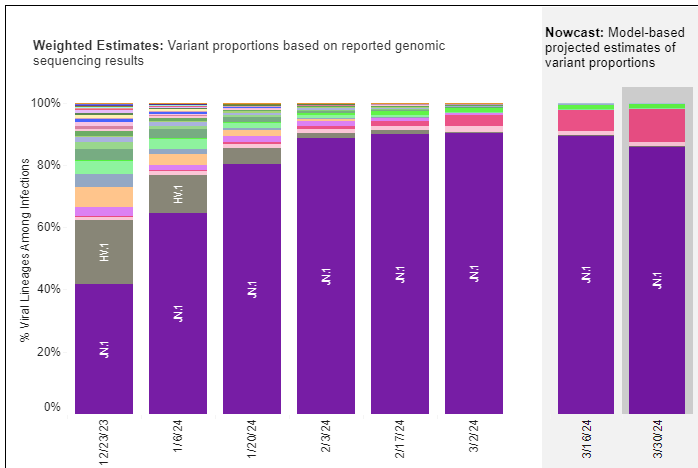
JN.1 and its progeny are still the main variants. JN.1 + FLiRT mutation has now been seen in 27 countries, but is still at very low levels. It is expected to take over in a few weeks to months.
This week, an article in the New England Journal of Medicine showed no significant difference in time until resolution of symptoms between those taking Paxlovid (12 days) and those taking placebo (13 days). However, Paxlovid did decrease the risk of hospitalization and of death. The study had limitations in that the median age of people in this study was 42 years old and only 5% of participants were over age 65.
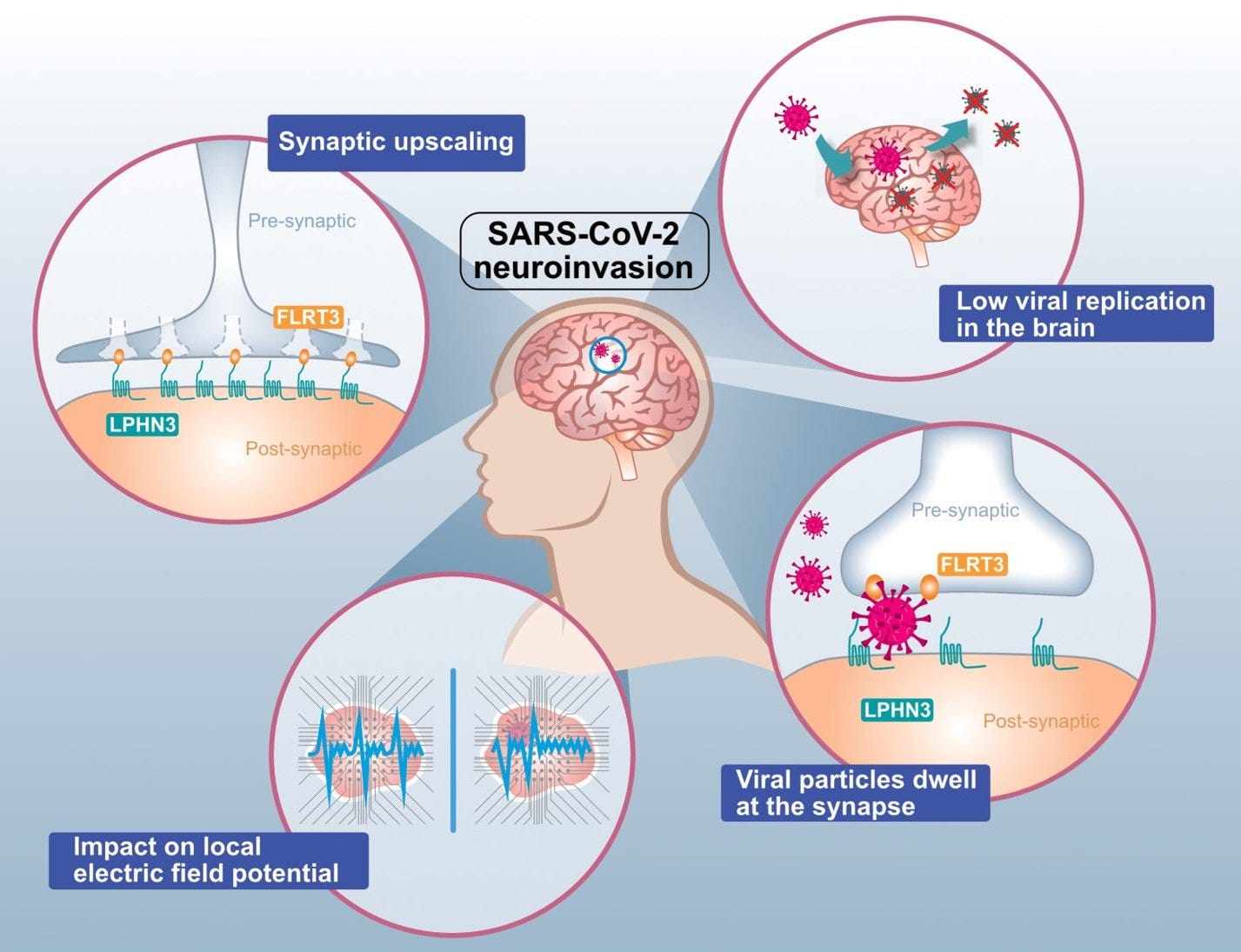
There were two interesting studies on acute COVID infection and the brain this week. The first study shows that even though there are low levels of SARS-2 virus particles in the brain, the virus particles tend to hang out in the synapses between nerves disturbing normal electrical messaging between neurons. The authors concluded, “Here we show that exposure to SARS-CoV-2 can perturb neuronal synapse morphology, modulate the synaptosome landscape and interfere with local electrical field potential.”
From: https://rdcu.be/dCNLx
A second article looks at mast cells in the brain. SARS-CoV-2 spike protein triggers mast cells to degranulate histamine and inflammatory mediators in the brain. This causes damage to tight junctions between endothelial cells in small brain blood vessels. It also causes microglia to release inflammatory factors (IL-6, IL-1β, and CCL20) and induces microglia activation and proliferation.
Long COVID
Nature magazine featured people with Long COVID who are helping to design research studies to cure themselves. Pharmacist Martha Eckey has Long COVID. She designed a survey for people with Long COVID and those with ME/CFS about 150 medications and supplements to see which helped. More than 4,000 people with Long COVID and/or ME/CFS responded to the survey. Supplements that gave some symptomatic relief included nattokinase, serrapeptase or lumbrokinase. Beta blockers and the heart-failure medication Corlanor (ivabradine) were particularly effective for Long COVID patients, as was low dose naltrexone. The Open Medicine Foundation now plans to do a double-blind, randomized, placebo-controlled clinical trial of low-dose naltrexone (LDN) and pyridostigmine. Others are planning to test immunomodulatory drug baricitinib.
Elite athletes and sports medicine doctors test blood lactate levels to check limits of anaerobic metabolism. Using blood lactate measurements, people with Long COVID or ME/CFS may be able to better pace themselves to avoid post-exertional malaise (PEM) crashes according to a new article.
A new JAMA article from Sweden states that “cautious exercise rehabilitation should be recommended to prevent further deconditioning among patients with PCC.” However, these recommendations were based on only 30 Long COVID patients, of which only 13% had POTS (Postural Orthostatic Tachycardia Syndrome). The results cannot (and should not) be applied to most Long COVID patients.
Many other studies have shown that exercise can actually hurt people with Long COVID. Rob Wust lab’s landmark study showed that in Long COVID patients with post-exertional malaise, exercise induces severe tissue damage and even muscle necrosis. Skeletal muscle mitochondrial function and metabolism were abnormal in patients with Long COVID and this worsened when post-exertional malaise (PEM) was triggered with exercise. As Rob Wust tweeted in January, “Intense exercise is not good for patients with long COVID!”
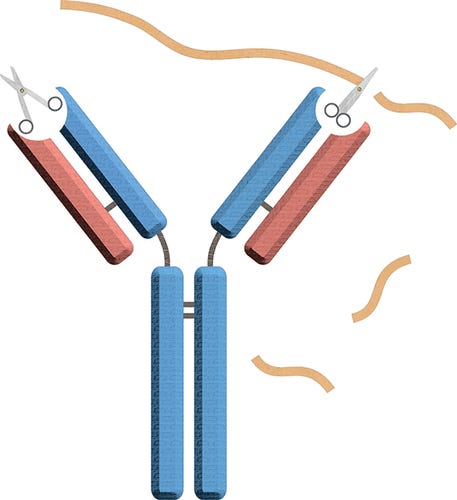
Health Rising posted an article this week entitled “Copaxone - Could a Multiple Sclerosis Drug Help with ME/CFS?” Ron Davis’ lab found that half of MECFS patients that they tested had catalytic autoantibodies that break down myelin in the exact same pattern as in Multiple Sclerosis (MS). Myelin is the protective sheath that wraps around nerves insulating them to allow electrical impulses (messages) to be sent from one nerve to the next quickly. The Davis lab also tested an multiple sclerosis immunomodulator drug called glatiramer acetate (Copaxone) in vitro and found that it inhibited the ME/CFS antibody digestion of myelin basic protein. “Postpandemic research has also provided several reports of demyelination in COVID-19.” However, not as much demyelination is seen in ME/CFS as is seen in multiple sclerosis and it is “possible that the amount of antibody in ME/CFS is not as high as in MS.”
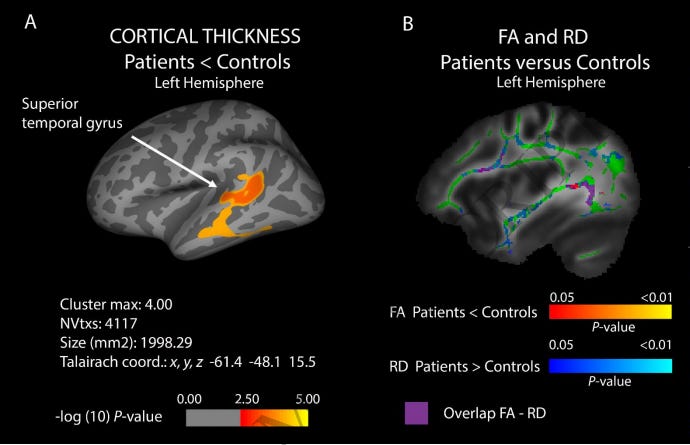
A group from Barcelona looked at 53 relatively young people with post-COVID conditions (PCC or Long COVID) at 1.8 years after COVID infection using both neuropsychological testing to identify cognitive changes and a specialized MRI of the brain. The most common cognitive impairments were in memory, executive function and in attention. Impaired memory in Long COVID correlated with reduced cortex thickness in the left parahippocampal region and the right caudal-middle-frontal regions of the brain.
Mónica Muñoz-López’s group from Albacete, Spain looked at brain and cognitive changes in 83 Long COVID patients as compared to 22 COVID infection recovered controls. Long COVID patients had diffuse damage in the white matter of the brain, especially in the temporal lobe that was associated with poor cognition. “Correlations between cognitive status and brain abnormalities revealed a relationship between altered connectivity of white matter regions and impairments of episodic memory, overall cognitive function, attention and verbal fluency.”
Figure 2: Differences in cortical thickness and underlying white matter between patients and controls in the left posterior superior temporal region. https://buff.ly/43Tip79
Clinical trials
A double blind randomized clinical trial showed that Lactoferrin provided no benefit to reduce fatigue, other symptoms of Long COVID or physical functioning. Vyvgart (Efgartigimod), an antibody fragment made to reduce pathogenic IgG by binding the Fc receptor, was found to be safe and effective for treating Sjogren’s Disease in a Phase 2 clinical trial. Vyvgart is also being tested for post-COVID POTS and results are expected within the next few months. Shionogi, maker of antiviral medicine Ensetrelvir, will be collaborating with Osaka University to do clinical research on preventing Long COVID. The PolyBio Spring Symposium will take place online on May 17th and investigators will be giving updates on their research projects.
In non-COVID news, highly pathogenic avian influenza (HPAI) H5N1 was found in dairy cattle this week in several states including Texas, Kansas, Michigan and New Mexico. One human who worked with the infected cattle also became infected in addition to several cats on one of the dairy farms. Virologist Angie Rasmussen commented “Particularly worrisome is the fact that this human case was limited to mild conjunctivitis. That’s good for the person who got H5N1. I’m glad they didn’t become seriously ill. But it’s not good for preventing spillover. Mild cases may not be recognized & isolated.”
Eric Topol MD reviewed how artificial intelligence (AI) can detect Type 2 diabetes, heart ejection fraction and 10 year risk of heart attack and stroke from a simple chest Xray. This week, the FDA approved an AI algorithm to detect heart failure embedded in a digital stethoscope from Eko Health. Eko worked with Mayo Clinic to create the device. Eko’s stethoscopes already use AI algorithms to detect atrial fibrillation and a structural heart murmur. A smartphone app was found to reliably diagnose Frontotemporal lobar degeneration (FTLD) remotely. Giving mice Lixisenatide, an older glucagon-like peptide-1 receptor agonist for diabetes, was found to be neuroprotective against Parkinson's disease.
A 4.8 earthquake centered in New Jersey shook New York City this week. The Empire State Building tweeted to let everyone know that it was fine.
Have a good rest of your weekend,
Ruth Ann Crystal MD
COVID news notes:
US Variant tracker: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
Variants around the world:
https://outbreak.info/
World wastewater maps (reflects COVID cases): https://www.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082
NEW: 3/27/24 WHO launches CoViNet: a global network for coronaviruses (SARS-2, MERS, etc)
https://www.who.int/groups/who-coronavirus-network
CDC COVID data tracker: https://covid.cdc.gov/covid-data-tracker/index.html#datatracker-home
Test positivity 4.0%
Emergency Dept visits: -21.1%
Hospitalizations: -13.9%
Deaths -16.7%
CDC COVID Hospitalizations (blue) and Emergency Room (orange) visits tracker: https://covid.cdc.gov/covid-data-tracker/index.html#trends_weeklyhospitaladmissions_7dayeddiagnosed_00
Weekly ED visits for respiratory illnesses, by age and disease: https://www.cdc.gov/ncird/surveillance/respiratory-illnesses/index.html
US Wastewater Monitoring:
CDC wastewater reporting: https://www.cdc.gov/nwss/rv/COVID19-nationaltrend.html
CDC wastewater map: https://www.cdc.gov/nwss/rv/COVID19-currentlevels.html
Biobot: https://biobot.io/data/
National SARS-CoV-2 data from Sara Anne Willette: https://iowacovid19tracker.org/
New Mexico has very high levels of virus in wastewater. Missouri has moderate levels.
Wastewater SCAN:
https://data.wastewaterscan.org/
California state view https://buff.ly/3YObiul
Sewer Coronavirus Alert Network (SCAN) project by Stanford University:
Santa Clara County wastewater: https://covid19.sccgov.org/dashboard-wastewater
Marin county: https://coronavirus.marinhhs.org/surveillance
CDC Respiratory vaccination trends: https://www.cdc.gov/respiratory-viruses/data-research/dashboard/vaccination-trends-adults.html
JP Weiland: https://twitter.com/JPWeiland
https://twitter.com/JPWeiland/status/1776381105353969994
April 5th update: Now at low transmission levels, slight decline from last week.
Still some time until JN.1 with FLiRT take hold.
245,000 new infections/day
~2.76 avg total infections per capita across the US
1 in every 135 people currently infected
Michael Hoerger modeling: http://pmc19.com/data/, https://twitter.com/michael_hoerger
Variants
JN.1.+ FLiRT:
https://twitter.com/Mike_Honey_/status/1772612527525884348
Acute COVID infections, General COVID info
4/4/24 Frontiers in Cellular and Infection Microbiology (Guangzhou): Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia https://buff.ly/3PSn03T
"the role of Mast Cell (MC) activation in SARS-CoV-2–induced neuroinflammation.
We found that
(1) SARS-CoV-2 infection triggered MC accumulation in the cerebrovascular region of mice
(2) spike/RBD (receptor-binding domain) protein–triggered MC activation induced inflammatory factors in human brain microvascular endothelial cells and microglia;
(3) MC activation and degranulation destroyed the tight junction proteins in brain microvascular endothelial cells and induced the activation and proliferation of microglia.
These findings reveal a cellular mechanism of SARS-CoV-2–induced neuroinflammation.
Figure 5 Graphical abstract.
MC degranulation causes inflammation in brain microvascular endothelial cells and microglia.
The treatment with SARS-CoV-2 spike protein triggers MC degranulation, and the degranulated component such as histamine induces the inflammatory factors CXCL5, SAA2, SERPINA1 in human brain microvascular endothelial cells, and reduced the tight junction proteins of OCLN, ZO-1, and JAM2;
MC degranulation also increases the expression of inflammatory factors IL-6, IL-1β, and CCL20 in microglial cells, and induces the activation and proliferation of microglia.
https://twitter.com/Gaudinlab/status/1773666956605849944
Link to article: https://rdcu.be/dCNLx or https://t.co/7ZJ8ivnbz6
3/28/24 Nature Microbiology: Brain exposure to SARS-CoV-2 virions perturbs synaptic homeostasis https://buff.ly/3PLrSYr
4/3/24 CIDRAP: Wastewater testing near homeless camps shows COVID-19 viral mutations https://buff.ly/3VP6upc
water near encampments outside Las Vegas was sampled from December 2021 through July 2022.
Pediatrics
4/3/24 PLOS One: Ventilation during COVID-19 in a school for students with intellectual and developmental disabilities (IDD) https://buff.ly/4aBVtLK
Correlation of classroom ventilation (air exchanges per hour (ACH)) and exposure to CO2 ≥1,000 ppm with the incidence of SARS-CoV-2 over a 20-month period in a specialized school for students with intellectual and developmental disabilities (IDD).
Cleaner air in schools was associated with reduced COVID infections in students.
There was a statistically significant correlation between the total time of room CO2 concentrations ≥1,000 and SARS-CoV-2 cases in an IDD school.
Merv-13 filters appear to decrease the incidence of SARS-CoV-2 infection. This research partnership identified areas for improving in-school ventilation.
Antiviral treatments
4/4/24 CIDRAP: Among fully vaccinated, study shows Paxlovid does not shorten symptoms in younger patients https://buff.ly/3U56XCh
The study was conducted from July 2021 to July 2022.
With Paxlovid, COVID infection symptoms did not go away any faster than placebo, but Paxlovid treatment did decrease hospitalizations and death from any cause.
The trial was notable for including younger participants: The median age was 42 years, and only 5% were 65 years of age or older.
"Can we really say an unvaccinated 18-year-old has the same risk factor as a vaccinated 89-year-old? I don't think so." Osterholm
4/3/24 NEJM: Nirmatrelvir for Vaccinated or Unvaccinated Adult Outpatients with Covid-19 https://buff.ly/3VLj34v
n = 654 Paxlovid (nirmatrelvir–ritonavir) vs 634 who took placebo. August 2021 to July 2022.
In people at standard or high risk for severe COVID infection, there was no significant difference in time until resolution of symptoms between those taking Paxlovid (12 days) and those taking placebo (13 days). However, Paxlovid did decrease the risk of hospitalization and of death.
Long COVID
4/2/24 Nature: Long COVID still has no cure — so these patients are turning to research https://buff.ly/4aeXMoz
Lisa McCorkell co-founded the Patient-Led Research Collaborative (PLRC), to design, provide advice on and even fund basic and clinical research into long COVID and other chronic illnesses.
Martha Eckey, a pharmacist in Minneapolis, designed a survey called TREAT ME, which asked people with long COVID and those with ME/CFS, about 150 medications and supplements. More than 4,000 people responded.
Eckey’s results, which have not yet been published in a peer-reviewed journal, show that of 668 respondents with long COVID, between 40% and 70% found some symptom relief when taking the supplements nattokinase, serrapeptase or lumbrokinase, individually or in combination Putrino to do a 120-person study on lumbrokinase in the coming months, and has involved patients at every step of its development.
Some treatments revealed by the survey as most effective for long COVID were drugs such as beta blockers and the heart-failure medication Corlanor (ivabradine).
Eckey also found that a number of individuals reported relief after taking low dose naltrexone.
Open Medicine Foundation to do a double-blind, randomized, placebo-controlled clinical trial will explore low-dose naltrexone (LDN) and another drug, pyridostigmine, which is used to treat an autoimmune disorder that affects voluntary muscle movements.
Hannah Davis and Jaime Seltzer, director of scientific and medical outreach at the non-profit organization ME Action in Santa Monica, California. Test baricitinib, an immunomodulatory drug. Wes Ely.
“Every research trial that we run, we involve the patient community in the protocol,” Putrino says. This includes taking their advice on what trials should be prioritized, what symptoms to assess, how many clinic visits to require and what the testing environment should be like, to minimize the risk of exacerbating their symptoms, he says.
Elite athletes and sports medicine doctors test blood Lactate levels to check limits of anaerobic metabolism. Using blood lactate measurements, people with Long COVID or ME/CFS may be able to better pace themselves to avoid post-exertional malaise (PEM) crashes.
3/30/24 Current Problems in Cardiology (Rae Duncan et al.): Attenuating Post-exertional Malaise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (MECFS) and Long-COVID: Is Blood Lactate Monitoring the Answer? https://buff.ly/3vDWW5E
Lactic acid is a by-product of anaerobic metabolism. Blood lactate has long been used in sports medicine as a surrogate marker of anaerobic thresholds and is commonplace in elite sports.
Lactate monitoring presents an opportunity to support those living with ME/CFS and Long COVID, by allowing patients and practitioners to determine the intensity and anaerobic contribution to everyday tasks which could aid the development of pacing strategies that prevent PEM/PESE.
Problematic new article on exercise in Long COVID:
4/4/24 JAMA: Exercise Intolerance in Patients With Post-COVID Condition https://buff.ly/3J7W4t4
This study is too small with only 30 Long COVID patients vs 31 controls
https://twitter.com/postviraltrials/status/1776088020246008299
https://twitter.com/EricTopol/status/1775908851738644622
4/3/24 Health Rising: Copaxone - Could a Multiple Sclerosis Drug Help with ME/CFS? https://buff.ly/3vFhCtS
Ron Davis’ lab found that half of MECFS patients that they tested had catalytic autoantibodies that break down myelin in the exact same pattern as in Multiple Sclerosis (MS). Myelin is the protective sheath that wraps around nerves insulating them to allow them to increase the speed of electrical impulses (messages) sent from one nerve to the next. The Davis lab also tested an multiple sclerosis immunomodulator drug called glatiramer acetate (Copaxone) and found that it also inhibits the ME/CFS antibody digestion of MBP.
11/27/23 Biochemistry (Ron Davis): Catalytic Antibodies May Contribute to Demyelination in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) https://buff.ly/47S7ITc
Like in multiple sclerosis, half of ME/CFS patients tested by Ron Davis and colleagues showed catalytic autoantibodies (abzymes) that cause the breakdown of myelin basic protein (MBP).
“We also tested glatiramer acetate (copaxone), an FDA approved immunomodulator to treat multiple sclerosis, and found that it inhibits ME/CFS antibody digestion of MBP.
“Furthermore, we found that aprotinin, which is a specific serine protease inhibitor, specifically prevents breakdown of MBP while the other classes of protease inhibitors had no effect. This coincides with the published literature describing catalytic antibodies as having serine protease-like activity.
“Postpandemic research has also provided several reports of demyelination in COVID-19. Because COVID-19 has been described as a trigger for ME/CFS, demyelination could play a bigger role in patient symptoms for those recently diagnosed with ME/CFS.
Therefore, by studying proteolytic antibodies in ME/CFS, their target substrates, and inhibitors, a new mechanism of action could lead to better treatment and a possible cure for the disease.”
PolyBio Spring Symposium, May 17th, 9am PT, 12pm ET
https://us02web.zoom.us/webinar/register/WN_Od4HsQn-Thq87EreSse-6w#/registration
4/2/24
https://twitter.com/jenbrea/status/1775332860427461002
@JenBrea: Favorite #MECFS / #longCOVID / #POTS / #EDS studies from the past year? (Trying to catch up.)
3/25/24 Devex: UN relief czar says long COVID is forcing him to step down https://buff.ly/3TzhNic
Martin Griffiths, the United Nations chief emergency relief coordinator has Long COVID and has to stop his global work.
Office for the Coordination of Humanitarian Affairs at the United Nations
3/24/24 People Magazine (interview w/Dr. Al-Aly): COVID Linked to Lower IQ, Poor Memory and Other Negative Impacts on Brain Health https://buff.ly/3UaH7gl
Great article with references to recent data on COVID's negative effects on the brain.
Findings from a webinar entitled “Long COVID’s Impact on Patients, Workers & Society” reviewed Long COVID’s etiology, symptoms, treatments and societal impacts. Misinformation and public health strategies were also discussed.
3/22/24 Medicine: Long COVID’s Impact on Patients, Workers, & Society: A Review https://buff.ly/3xkqmGk
Kevin T. Kavanagh. Health Watch USA, Lexington, KY (e-mail: kavanagh.ent@gmail.com)
November 1, 2023, the webinar entitled “Long COVID’s Impact on Patients, Workers & Society” brought together international experts to share information regarding long COVIDs’ etiology, presentation, treatment, and societal impact (Table 1). In addition, the public’s hesitancy in adopting public health strategies along with the inhibiting effects of organized disinformation were discussed.
“Key points
The best way to prevent long COVID is to not develop COVID-19.
Neurological and immunological manifestations of long COVID can have a profound impact on children and adults.
Neurological sequelae can present as brain fog, cognitive disorders, personality changes, and executive dysfunction. The prefrontal cortex is particularly susceptible.
Immunological sequelae can present as autoimmune diseases and increase susceptibility to common diseases.
Approximately 11% of acute SARS-CoV-2 infections develop long COVID of these patients, 26% have difficulty with day-to-day functions.
Rehabilitation involves a “low and slow” process and post-exertional malaise can occur if physical or mental activities are initiated too quickly.
Vaccinations even after developing acute COVID-19 can help prevent or mitigate the symptoms of long COVID.”
A group from Spain looked at 53 relatively young people with post-COVID conditions (PCC or Long COVID) at 1.8 years after COVID infection using both neuropsychological testing to identify cognitive changes and a specialized MRI of the brain. The most common cognitive impairments were in memory, executive function and in attention. Impaired memory correlated with reduced brain cortex thickness in the left parahippocampal region and the right caudal-middle-frontal regions of the brain.
4/4/2024 American Journal of Neuroradiology (early 4/2024 edition): Reduced Cortical Thickness Correlates of Cognitive Dysfunction in Post-COVID-19 Condition (PCC, Long COVID): Insights from a Long-Term Follow-up https://buff.ly/3W4DYjx
N = 53 with Long COVID
3T brain MR imaging with T1 and FLAIR sequences obtained a median of 1.8 years after COVID infection to investigate brain volumes and cortical thickness and their associations with cognitive function
Neuropsychological testing to assess cognitive domains
“cognitive deficits were associated with changes in brain macrostructure, especially in the left parahippocampal region and the right caudal-middle-frontal region, possibly explaining the cognitive symptoms described by these participants.
The most common cognitive impairments objectified by COVID-19 with the PCC are in attention, memory, and executive functions.
We used FreeSurfer to measure cortical thickness based on intensity and continuity information from MR imaging volumes.
Impaired memory was related to reduced brain cortex thickness in the left parahippocampal region and the right caudal-middle-frontal region.
Mónica Muñoz-López’s group from Spain also looked at brain and cognitive changes in 83 Long COVID patients as compared to 22 COVID infection recovered controls. Long COVID patients had diffuse damage in the white matter of the brain, especially in the temporal lobe that were associated with poor cognition. “Correlations between cognitive status and brain abnormalities revealed a relationship between altered connectivity of white matter regions and impairments of episodic memory, overall cognitive function, attention and verbal fluency.”
4/2/24 Brain: Brain and cognitive changes in patients with long COVID compared with infection-recovered control subjects https://buff.ly/43Tip79
83 patients with Long COVID vs 22 controls who had recovered from COVID without symptoms. "48% of patients with Long COVID had episodic memory deficit, with 27% also impaired overall cognitive function, especially attention, working memory, processing speed and verbal fluency."
Compared to infection recovered controls, Long COVID patients had thinner cortex in a specific cluster centered on the left posterior superior temporal gyrus.
In addition, lower fractional anisotropy (FA) and higher radial diffusivity (RD) were observed in widespread areas of the patients’ cerebral white matter relative to these controls.
Correlations between cognitive status and brain abnormalities revealed a relationship between altered connectivity of white matter regions and impairments of episodic memory, overall cognitive function, attention and verbal fluency.
Patients with neurological Long COVID suffer brain changes, especially in several white matter areas, and these are associated with impairments of specific cognitive functions.
Compared to infection-recovered controls, Long Covid patients have more spread and diffuse damage in the white matter. Despite restricted focal points of brain changes in gray matter, white matter alterations, especially in the temporal lobe, were more diffuse and significantly associated with poor cognitive performance.
This study shows that patients with neurological Long COVID suffer brain changes, especially in several white matter areas, and these are associated with impairments of specific cognitive functions.
Figure 2: Differences in cortical thickness and underlying white matter between patients and controls in the left posterior superior temporal region.
Double blind RCT shows no difference in Lactoferrin versus placebo in Long COVID.
2024 ERJ: Effect of Lactoferrin treatment on symptoms and physical performance in Long-COVID patients: a randomized, double-blind, placebo controlled trial https://buff.ly/3IZN3lL
randomized, double-blind placebo-controlled trial in long-COVID patients
3 hospital visits (T0, T6, and T12 weeks) patient reported outcome measures (PROMs) were collected, physical performance tests were performed, and blood was drawn.
Although both long-COVID arms showed improved clinical outcomes at T6, the improvement did not continue until T12. Lactoferrin provided no benefit in terms of fatigue, other PROMs or physical functioning.
https://twitter.com/postviraltrials/status/1774063959340937460
3/26/24 Argenx Advances Clinical Development of Efgartigimod in Primary Sjogren’s Disease https://buff.ly/49y531D
efgartigimod will advance to Phase 3 in adults with primary Sjogren’s disease (SjD), following the analysis of topline data from the Phase 2 RHO study. Detailed results will be presented at a future medical meeting.
The decision to advance the clinical development of efgartigimod in Sjogren’s disease (SjD) was supported by the safety, efficacy and biomarker results from the study.
https://twitter.com/DavidFajgenbaum/status/1768288604944531707
Job posting at Every Cure: https://www.linkedin.com/jobs/view/3841097939/
https://chasingmycure.com/contact/
3/1/24 Shionogi Press Release https://buff.ly/49jziJe
Shionogi and Osaka University Establish a New Joint Research Lab on Post-COVID-19 Condition (Long COVID)
Shionogi makes Ensetrelvir
Conducting clinical research aimed at establishing methods to prevent Long COVID.
AI:
4/1/24 MedCity News: ‘Garbage In Is Garbage Out’: Why Healthcare AI Models Can Only Be As Good As The Data They’re Trained On https://buff.ly/3J4bRZU
https://twitter.com/EricTopol/status/1774804498051158186
3/31/24 Eric Topol MD: Opportunistic A.I. for Medical Scans https://buff.ly/4aC6LzH
Using a simple Chest Xray and AI to detect Type 2 diabetes, heart ejection fraction and 10 year risk of heart attack and stroke.
3/20/24 Stanford Med LIVE (video): The State of AI in Healthcare and Medicine https://buff.ly/4ajuR2F
Leaders of Stanford Medicine discuss artificial intelligence in health and medicine; its usefulness in research, education and patient care; and how to responsibly integrate the technology.
Other news:
4/3/24 NEJM: Trial of Lixisenatide in Early Parkinson’s Disease https://buff.ly/3TIDL2n
Mice given Lixisenatide, a glucagon-like peptide-1 receptor agonist for diabetes, was neuroprotective against Parkinson's in mice.
"In participants with early Parkinson’s disease, lixisenatide therapy resulted in less progression of motor disability than placebo at 12 months in a phase 2 trial but was associated with gastrointestinal side effects."
No progression of motor disability in the Rx group for 12 months.
4/2/24 STAT News: FDA clears digital stethoscope company’s AI algorithm for heart failure https://buff.ly/3xjvzhD
Congrats Eko Health!
4/2/24 STAT news: A nation with too few pediatricians could see health care costs soar https://buff.ly/3PLqjtI
4/1/24 CIDRAP: Avian flu (H5N1) infects person exposed to sick cows in Texas https://buff.ly/4aht2Dj
4/2/24 CIDRAP: Tests confirm avian flu on New Mexico dairy farm; probe finds cats positive https://buff.ly/3U4NdO3
https://twitter.com/angie_rasmussen/status/1775518238014845403
Dr Angie Rasmussen:
“So the H5N1 virus that spilled over from cows to a human has acquired a mutation associated with mammalian adaptation.
(Human H5N1 case in Texas matches other Texas sequences plus
PB2 E627K mutation)
This is what RNA viruses do when faced with a new host: adapt or die.
To prevent further adaptation, we need to stop further cross-species transmission.
Particularly worrisome is the fact that this human case was limited to mild conjunctivitis.
That’s good for the person who got H5N1. I’m glad they didn’t become seriously ill.
But it’s not good for preventing spillover. Mild cases may not be recognized & isolated.”
https://twitter.com/PeacockFlu/status/1775512325967032404
4/3/24 Tom Peacock: Regarding H5N1 virus spillover to mammals
“Might do an update to this thread at some point in light of recent developments... think there's some interesting further developments in some of the other mammals as well that might have gone under the radar (particularly the sealions)”
4/1/24 Healio: Low-dose aspirin ‘significantly’ reduced hepatic fat in MASLD by more than 10% vs. placebo https://buff.ly/3TZNClW
Data derived from: Simon TJ, et al. JAMA. 2024;doi:10.1001/jama.2024.1215.
4/1/24 JAMA: Smartphone Cognitive Testing for Frontotemporal Lobar Degeneration https://buff.ly/3VEv0sX
3/29/24 The Hill: STDs have risen among adults 55 and older: CDC https://buff.ly/4cFFrSV
“Researchers think misconceptions about STDs among older Americans are contributing to the rise.”
7x more Gonorrhea, 4x more Chlamydia and 8x more Syphilis in people age 55+ since 2010.
3/29/24 HealthDay: High-Strength Lidocaine Skin Creams Can Cause Seizures, Heart Trouble, FDA Warns https://buff.ly/3U1Lj1u
"Products containing lidocaine over 4% can contribute to health problems like an irregular heartbeat, seizures and breathing difficulties, the FDA explained. They also can interact with other medications or supplements a person is taking."
"The FDA is particularly concerned if these products are applied over large areas of skin for prolonged periods of time, especially if the skin is irritated or broken."
3/28/24 FT (John Burn-Murdoch): Why family-friendly policies don’t boost birth rates https://buff.ly/43VIYsF
https://twitter.com/LaurenBerson/status/1774152468139532353
Copyright, Ruth Ann Crystal MD






































Thank you for your always excellent and easy to understand review of important medical news!
All useful content and a laugh at the end for the tweet from the Empire State Building. Thank you 🙏🏼