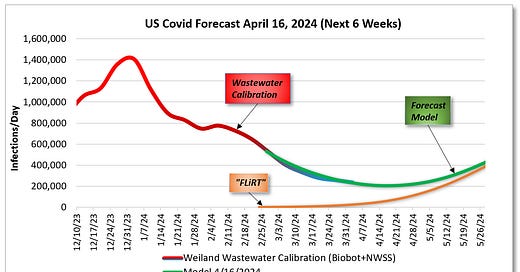
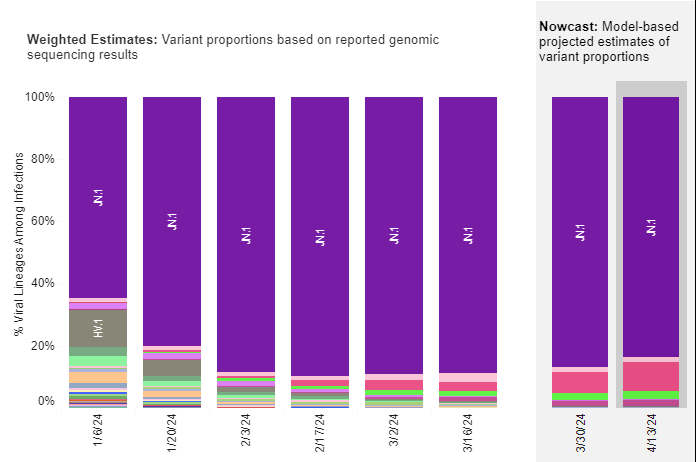
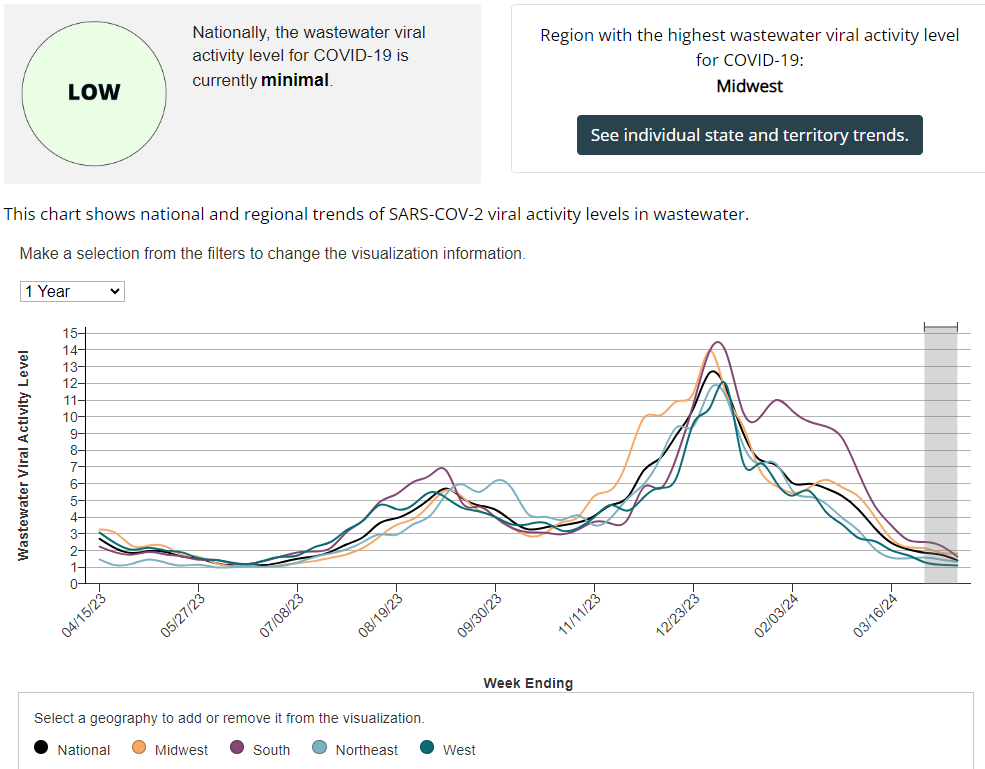
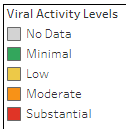
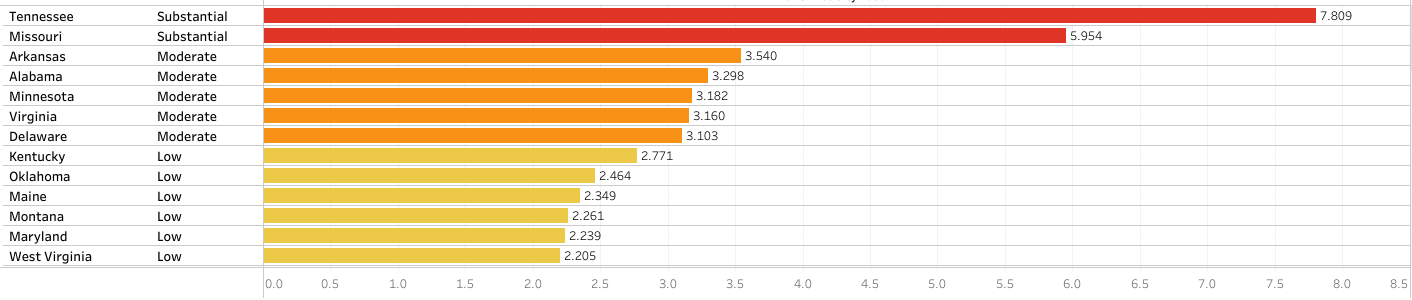
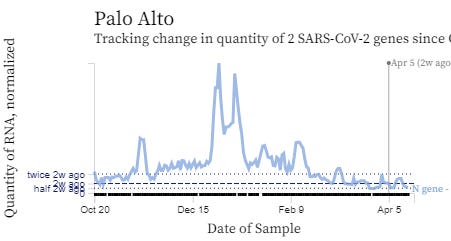
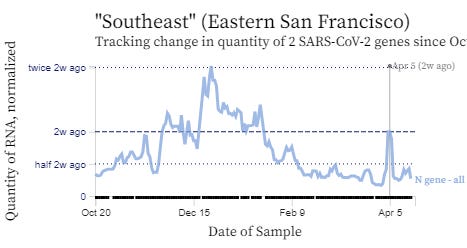
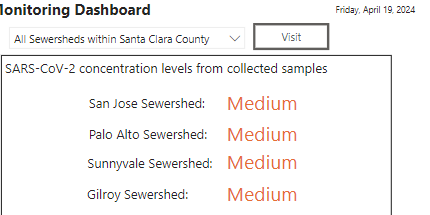
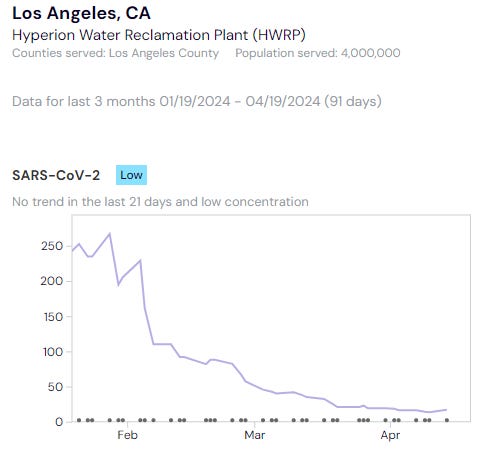
Wastewater levels are “LOW” across the US and hospitalizations, emergency department visits and deaths from COVID have decreased even more. JN.1 and its descendants are responsible for almost all COVID cases now. In the Bay Area, Santa Clara county is in the “MEDIUM” level for SARS-CoV-2 in wastewater. Stanford had a huge spike of wastewater virus a few days ago that has now resolved. There are also HIGH viral wastewater levels of SARS-CoV-2 in Mill Valley, and MEDIUM levels in Sausalito and San Rafael. Although numbers are low nationally, I personally know four people who have had a COVID infection in the last week. According to JP Weiland, about 1 in every 164 people is currently infected and there are about 200,000 new COVID cases per day across the United States. You can see wastewater levels for your county by searching on Wastewater SCAN.
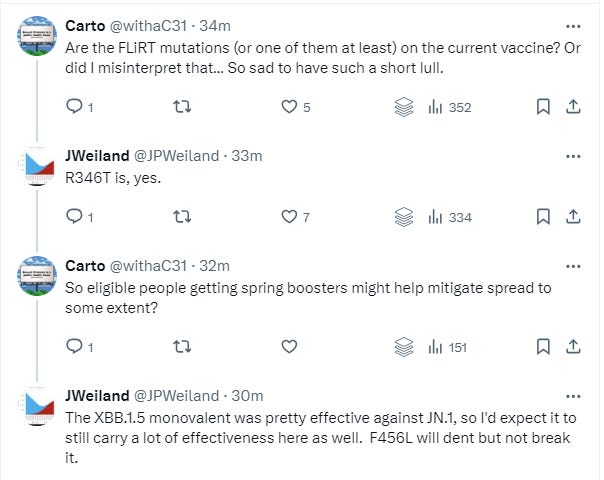
Although we are at low virus levels for the U.S. now, variant hunters on Twitter have alerted that new JN.1 descendants with the FLiRT mutation (subvariants KP.3, KP.2, KS.1, KP.1.1) have a significant growth advantage over JN.1 and therefore may cause another COVID wave(let) in the next 6 weeks. According to Eric Topol MD and JP Weiland, JN.1 + FLiRT subvariants will probably not cause a very large wave, since our collective immune systems have seen the FLiRT mutation in past variants and since the JN.1 wave just recently happened. The latest COVID vaccine (against XBB.1.5) does provide protection against JN.1 for hospitalization and death for at least several months. We do not know yet if this vaccine will work against JN.1 + FLiRT subvariants yet, but the feeling is that the XBB.1.5 vaccine should offer at least some protection. Seniors and immunocompromised people should get their second dose of the XBB.1.5 vaccine soon.
Figure: Ben Murrell shows the growth advantage of JN.1 + FLiRT subvariants (KP.3, KP.2, KS.1, KP.1.1)
Acute COVID infections, General COVID info
An eye-opening article came out showing that airborne SARS-CoV-2 virus can linger in a room and can infect others almost 5 hours after an infected person leaves a room. The authors used whole genome sequencing (WGS) and discovered that "genetically identical SARS-CoV-2 infected two patients who were admitted to a hospital room 1 hour, 43 minutes and 4 hours, 45 minutes after discharge of an asymptomatic infected patient".
Remdesivir made some news. Patients who did not require oxygen on admission to the hospital, but were treated with Remdesivir were found to have 25% reduction in in-hospital mortality compared to non-remdesivir treatment at 14 days and a 17% decrease in in-hospital mortality compared to non-remdesivir treatment at 28 days. The reduction in in-hospital mortality from giving Remdesivir at hospital admission was seen with all COVID variants.
The microbiome refers to the community of microorganisms (such as fungi, bacteria and viruses) that normally live in different parts of our bodies such as in the gastrointestinal system or the skin. A new study of the saliva of people with an acute COVID infection showed that the “oral microbiome and salivary cytokines may be predictive of COVID-19 status and severity.”
The SARS-2 virus can infect both exocrine and endocrine cells in the pancreas. A new study shows that COVID infection can cause increased insulin resistance, and even a loss of beta cells that make insulin. The loss of beta cells was associated with lower insulin production with islet amyloidosis and necrosis. Fortunately, vaccination against COVID was shown to help with glucose homeostasis by activating insulin receptor α and insulin receptor β. The authors noted "Overall, the cumulative risk of diabetes post-COVID-19 is closely tied to age, suggesting more attention should be paid to blood sugar management in elderly COVID-19 patients."
There were two other studies this week on age-dependent responses to SARS-2 infection. Older adults can be more susceptible to severe COVID infections. Using mass cytometry, serum proteomics, antibody assays, and transcriptional analysis, a group found that older age was associated with increased viral load, reduced ability to clear the virus, and dysregulation of immune signaling. Older adults also had higher expression of pro-inflammatory genes and proteins with severe COVID infections. In addition, herpes simplex virus and cytomegalovirus (CMV) were reactivated in the upper airways of older adults.
Another group looked at age-specific responses to SARS-CoV-2 infection in the nasal epithelial lining and found differences in the types of cells found in the nose. In children (<12 years old), a distinct goblet inflammatory cell was seen in the cells lining their noses, along with high interferon levels which stopped viral replication. In older adults (>70 years), nasal epithelial cells infected with SARS-2 showed an increase in basaloid-like cells, which helped the virus spread. Differing amounts of ACE2 and TMPRSS2 receptors were found in nasal epithelial cells in different age groups.
From: https://www.nature.com/articles/s41564-024-01658-1
Vaccines and antiviral medications
A modeling study of hybrid immunity from infection and from vaccination showed that the immunity wall from prior COVID infection does not last very long if people are not also vaccinated. Without vaccination, people can become reinfected with the same variant a few months after their first infection. Higher vaccination levels in a community provided a better immunity wall to stop secondary reinfections with the same variant.
Newer mutations help the SARS-2 virus to escape from some monoclonal antibodies that worked against prior variants. A group isolated 28 potent monoclonal antibodies and found that some of them regained the ability to neutralize newer variant BA.2.86. JN.1 is a descendant variant of BA.2.86.
A new study from Yale shows that neosporin ointment placed in the nose may help prevent COVID and the flu. Intranasal generic antibiotic neomycin increased interferon expression in the nose and protected mice and hamsters from COVID infection and from Influenza A. In humans, Neosporin was also found to increase antiviral interferon expression in the nose.
Long COVID
On April 15, Dr. Jeremy Faust interviewed NIH Director Monica Bertagnolli MD. During their conversation, Dr. Bertagnolli said that data shows that live SARS-CoV-2 virus can persist in tissues for months or even years. She also discussed the need for better antiviral medications to stop viral reservoirs in the body to possibly prevent Long COVID. This was the first time that someone from the government said that there are definitely viral reservoirs of SARS-CoV-2 in the body.
From their interview:
“Faust: I just want to follow up on something you said a moment ago about where this virus can be found in tissues. Are you suggesting that Long COVID is actually, the mechanism of that persistent live virus in humans?
Bertagnolli: We see evidence of persistent live virus in humans in various tissue reservoirs, including surrounding nerves, the brain, the GI [gastrointestinal] tract, to the lung.
Faust: OK. And you're saying this goes beyond the PCR's [polymerase chain reaction test] ability to get it in a regular swab so that we are missing chronic cases of SARS‑CoV‑2?
Bertagnolli: Correct. The virus can persist in tissues for months, perhaps even years.
Faust: OK. I think that's certainly one theory, but I'm not sure that that's settled. Is that fair? I mean, there's one thing between people who are autopsy, they died of viral sepsis, as opposed to people walking around. Is there a distinction there?
Bertagnolli: Our emerging data shows that the virus can persist into tissues in the long term, and I think that's really critical because it does help us think about possible ways to combat it, one being better antivirals. I think there's a lot of focus on developing new antivirals as a possible way of preventing long COVID, and the other might be more aggressive treatment with antiviral therapy upon initial diagnosis.”
This week, a study in Nature magazine stated that many people with Long COVID have resolution of immune dysregulation at 24 months. But, this study had many flaws. The authors’ definition of Long COVID was if someone had “fatigue, dyspnea or chest pain.” They did not study people with cognitive dysfunction, orthostatic intolerance, sleep disturbances or post-exertional malaise. More than 20% of their Long COVID patients were lost to follow-up. In addition, some people with Long COVID in the study were reinfected within the 24 months. While they said that immune dysregulation had resolved by 24 months, their data showed that people with Long COVID still had significant EBV T-cell exhaustion at 24 months. There are a lot of problems with this study and I anticipate that it will be retracted or changed.
Congratulations to Professor Akiko Iwasaki of Yale who was named one of TIME magazine’s 100 most influential people! Dr. Iwasaki studies how the immune system fights off viruses at mucosal surfaces. More recently, she has been investigating the pathophysiology of Long COVID and has been working on a mucosal vaccine against SARS-CoV-2.
ME/CFS and Long COVID
Elite athletes test their lactate levels to see if they have pushed their bodies into anaerobic respiration. A group from the UK suggests that lactate monitoring could also be used in people with ME/CFS and with Long COVID to see when they switch to anaerobic respiration to produce energy. Aerobic respiration takes place in the mitochondria and is very efficient at producing 38 ATP molecules from oxygen. In contrast, anaerobic respiration is not efficient- it only makes 2 ATP energy molecules and produces lactate as a waste product. People with Long COVID are not able to extract oxygen in their muscles and tissues like healthy people can, and therefore, they rely on anaerobic metabolism more often. Anaerobic metabolism in people with ME/CFS and Long COVID is thought to be one reason why they get post-exertional malaise from minimal movement or exercise. As ME Research UK stated, “monitoring blood lactate levels may provide an indication of abnormally increased anaerobic respiration in those with ME/CFS and Long COVID, but more research is needed.”
From: https://twitter.com/MEResearchUK/status/1779872308452065313
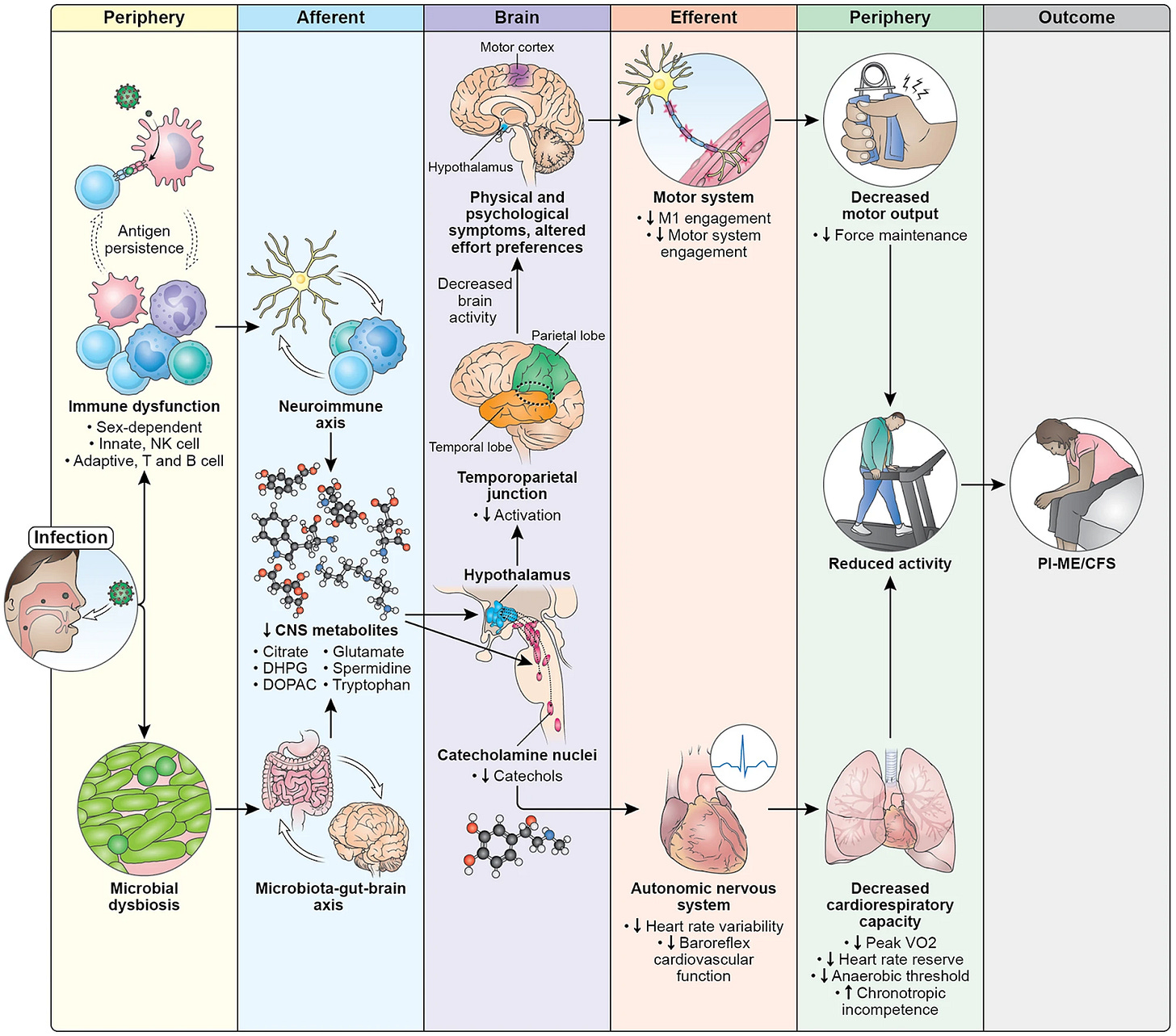
A new NIH initiative is trying to find out if Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) are the same disorder. Authors in Neurology Today reviewed an excellent article from Feb 21, 2024 from the NIH on post-infectious myalgic encephalomyelitis/ chronic fatigue syndrome (PI-ME/CFS). Dr. Avindra Nath stated “We believe these [ME/CFS and Long COVID] are virtually the same disease, … and they should be managed and studied in multidisciplinary clinics focused on post-infectious syndromes.”
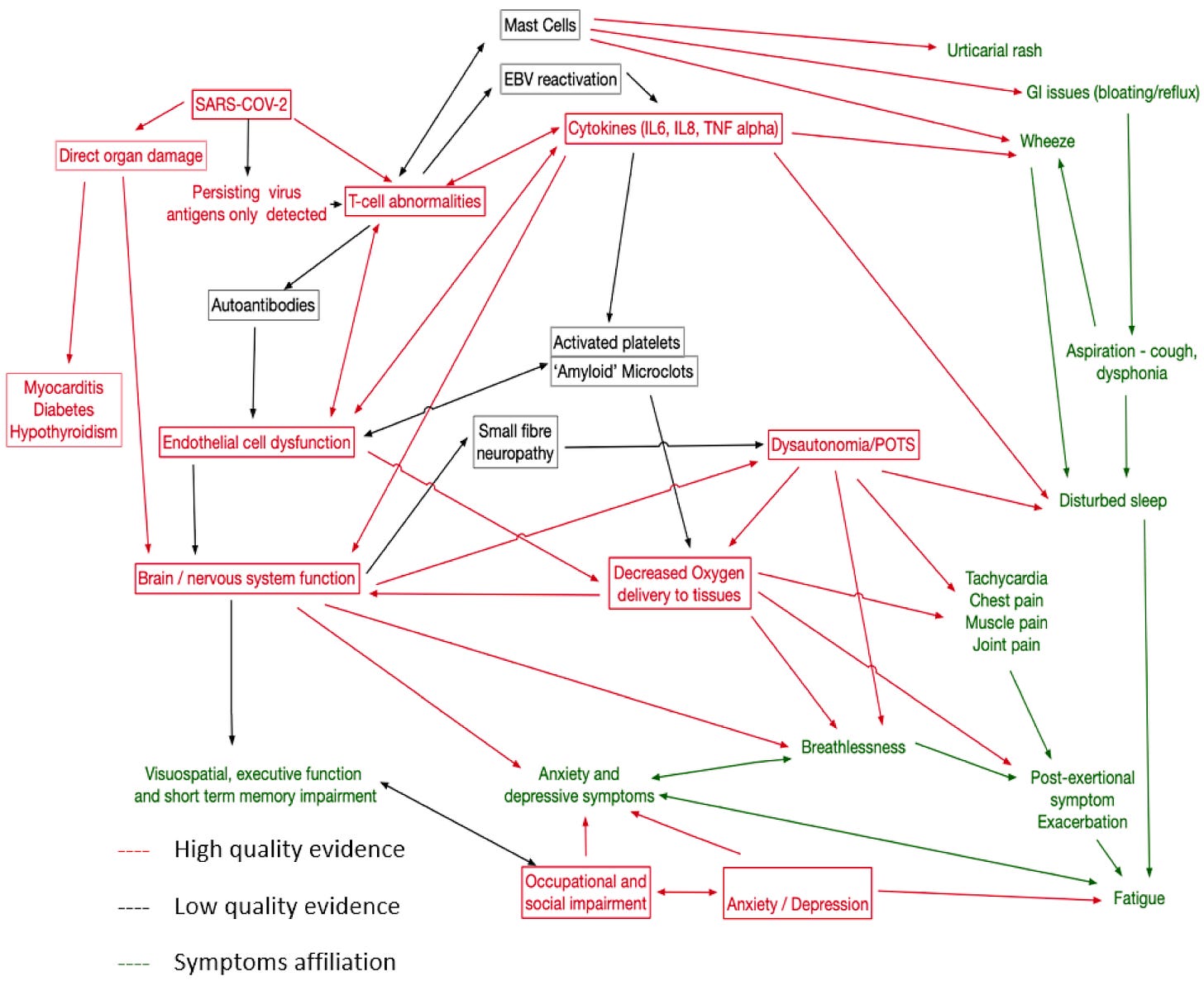
Below is the summary slide from the February article which shows COVID infection causes abnormal changes in the microbiome of the gut. This, in combination with immune dysfunction, leads to decreased metabolites that are used to make neurotransmitters in the brain. The lower levels of tryptophan and other metabolites causes several things to happen in the brain which then affect the heart and the skeletal muscles.
The catecholamine nuclei in the brain release less catechols, which affects the autonomic nervous system causing increased sympathetic function and decreased parasympathetic activity leading to decreased heart rate variability.
Abnormalities in the Hypothalamus decrease activation of the right temporoparietal junction which affects motor cortex function and leads to decreased motor strength.
Together, autonomic dysfunction of the heart and central motor dysfunction via the brain leads to decreased muscle strength which is seen as a decrease in physical activity and ability.
Fig. 10: Pathophysiology of PI-ME/CFS
ME/CFS
In August 2023, the Morten group from Oxford reported that using artificial intelligence and a single-cell Raman platform to evaluate Peripheral Blood Mononuclear Cells (PBMCs), they were able to distinguish ME/CFS with 91% accuracy. Specific Raman peaks also correlated with ME/CFS phenotypes. The Morten lab is now looking for a new PhD student to work on testing immune dysregulation in Lyme Disease and ME/CFS using Raman micro-spectroscopy.
Another recent study shows that low vasopressin secretion in ME/CFS may underlie symptoms such as orthostatic intolerance.
In non-COVID news, using artificial intelligence with machine vision during endoscopy doubled the detection of esophageal cancer and precancerous lesions. Stanford researchers are able to use lasers to scan the skin and create high-resolution, three-dimensional reconstruction of the cells in order to make noninvasive virtual biopsies. This could save people from getting an actual skin biopsy and scar in the future.
ACOG now recommends that because of “rapidly increasing rates of congenital syphilis, obstetrician–gynecologists and other obstetric care professionals should screen all pregnant individuals serologically for syphilis at the first prenatal care visit, followed by universal rescreening during the third trimester and at birth, rather than use a risk-based approach to testing.”
Regarding gestational diabetes, placental levels of IGFBP1 in early pregnancy were found to affect insulin sensitivity at 26 weeks gestation. A low level of IGF-1 gene expression in the placenta is linked to insulin resistance and gestational diabetes in pregnancy.
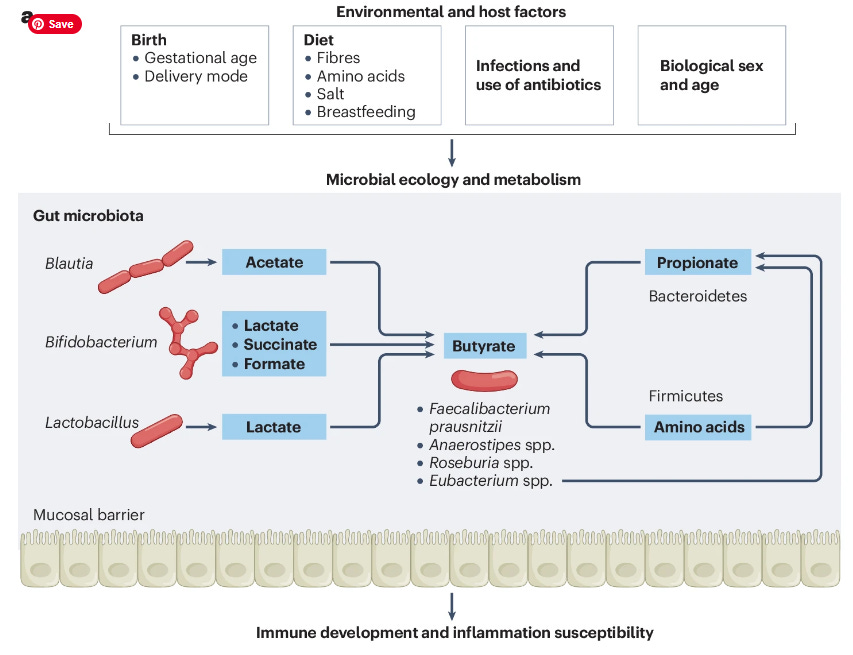
There was an interesting review in Nature Immunology on the effect of short-chain fatty acids (SCFA) such as butyrate on the gastrointestinal microbiome and on immunity. They discussed how certain environmental factors and diet can alter the microbiome which can affect both SCFA production and inflammation.
There were two articles on new treatments for early stage Parkinson’s disease to slow its progression. They included the GLP-1 receptor agonist drug Lixisenatide and a monoclonal antibody that binds α-synuclein called Prasinezumab.
I will be on vacation so my next newsletter will probably come out in 2 weeks.
Have a great week,
Ruth Ann Crystal MD
_____________________________
COVID news notes:
US Variant tracker: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
Variants around the world:
https://outbreak.info/
World wastewater maps (reflects COVID cases): https://www.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082
CDC COVID data tracker: https://covid.cdc.gov/covid-data-tracker/index.html#datatracker-home
Test Positivity 3.4%
ED visits down 19.9%
Hospitalizations down 13.8%
Deaths down 9.1%
CDC COVID Hospitalizations (blue) and Emergency Room (orange) visits tracker: https://covid.cdc.gov/covid-data-tracker/index.html#trends_weeklyhospitaladmissions_7dayeddiagnosed_00
US Wastewater Monitoring:
CDC wastewater reporting: https://www.cdc.gov/nwss/rv/COVID19-nationaltrend.html
CDC wastewater map: https://www.cdc.gov/nwss/rv/COVID19-currentlevels.html
Biobot: https://biobot.io/data/
National SARS-CoV-2 data from Sara Anne Willette: https://iowacovid19tracker.org/
Through April 16, 2024
Tennessee and Missouri are the only “substantial” level wastewater.
Wastewater SCAN (to see each state): https://data.wastewaterscan.org/
California statewide view https://buff.ly/3YObiul
Stanford had a huge spike of wastewater virus that has now resolved, followed by Mill Valley, Sausalito, and Las Gallinas, San Rafael
Sewer Coronavirus Alert Network (SCAN) project by Stanford University: https://soe-wbe-pilot.wl.r.appspot.com/charts
Santa Clara County wastewater: https://covid19.sccgov.org/dashboard-wastewater
Marin county: https://coronavirus.marinhhs.org/surveillance
CDC Respiratory vaccination trends: https://www.cdc.gov/respiratory-viruses/data-research/dashboard/vaccination-trends-adults.html
JP Weiland: https://twitter.com/JPWeiland
https://twitter.com/JPWeiland/status/1781447555475239149
Variants
https://twitter.com/JPWeiland/status/1780366091417424301
The best case scenario is that FLiRT has a muted takeover, and cases don't raise much. Worst case is this is the bottom of the lull for a while here.
https://twitter.com/withaC31/status/1780366822509797503
https://twitter.com/Mike_Honey_/status/1779979783251853450
4/18/24 Eric Topol MD: Are We FLiRTing With A New Covid Wave? https://buff.ly/3W5PV8r
“growth advantage of new variants that are derivatives of BA.2.86/JN.1, as posted by Ben Murrell, as seen below (KP.3, KP.2, KS.1, KP.1.1), all with double or more advantage.”
https://github.com/MurrellGroup/lineages/tree/2024-04-11?tab=readme-ov-file
“2 added spike mutations: F for L at position 456 and R for T at position 346, which has been nicknamed the FLiRT group of variants.”
My projection is that we could see a wavelet but not a significant new wave of infections as a result of the FLiRT variants in the next couple of months.
4/22/24 Christina Pagel (UK): Covid levels remain low but new variants are coming, as is bird flu https://buff.ly/3Wcai3Q
“Essentially, JN.1 has mutated further and several of its children have found mutations that help them spread much faster than their parent.
Together these are called the FLiRT group of variants.
In the US, the wave is forecast to start around May, but how large it will get is unknown.
Since these new FLiRT offshoots are more similar to JN.1, and we are heading into summer, hopefully any wave caused by these new subvariants will be smaller .”
Bird flu discussed also.
Acute COVID infections, General COVID info
4/5/24 American J of Infection Control: Evidence from Whole Genome Sequencing of Aerosol Transmission of SARS-CoV-2 almost Five Hours after Hospital Room Turnover https://buff.ly/3U5ZaTD
The authors used whole genome sequencing (WGS) and discovered that "genetically identical SARS-CoV-2 infected two patients who were admitted to a hospital room 1 hour, 43 minutes and 4 hours, 45 minutes after discharge of an asymptomatic infected patient". They concluded that airborne SARS-2 virus can infect others more than 4 hours after an infected person leaves the room.
Bay Area COVID safer shows
https://twitter.com/CovidSaferSF/status/1781078091676442800
(Palo Alto) Upcoming masked performances at Theatre Works Silicon Valley
"Tiger Style!" Sun., 4/21, 2 p.m.;
"Being Alive: A Sondheim Celebration," Fri., 6/14, 8 pm.; Sat., 6/15, 2 pm.; Sun. 6/23, 2 pm
More info: 877-662-8978 https://theatreworks.org/mainstage/
4/16/24 Open Forum Infectious Diseases: Remdesivir is associated with reduced mortality in patients hospitalized for COVID-19 not requiring supplemental oxygen https://buff.ly/3VYSgSA
58,188 remdesivir-treated patients were matched to 17,574 unique non-remdesivir patients.
At 14 days, Remdesivir treatment on admission to the hospital was associated with a statistically significant reduction of 25% in in-hospital mortality compared to non-remdesivir treatment.
At 28 days after admission, there was a 17% reduction in in-hospital mortality compared to non-remdesivir treatment.
The statistically significant reduction in in-hospital mortality from giving Remdesivir at hospital admission was seen across all variants.
Overall, 5.4% of remdesivir-treated and 7.3% of non-remdesivir patients died within 14 days, while 8.0% of remdesivir-treated and 9.8% of non-remdesivir patients died within 28 days. Remdesivir treatment was associated with a statistically significant reduction in in-hospital mortality compared to non-remdesivir treatment (14-day adjusted hazard ratio (aHR): 0.75, 95% confidence interval (CI): 0.68-0.83; 28-day aHR: 0.83, 0.76-0.90). This significant mortality benefit endured across the different VOC periods.
4/17/24 CIDRAP: Remdesivir tied to 25% lower risk of in-hospital death in adults with COVID and no added oxygen https://buff.ly/3Q7M1rR
"The antiviral drug remdesivir cut death rates 17% to 25% in adults hospitalized for COVID-19 who didn't require supplemental oxygen at admission, suggests a large US study."
3/25/24 PNAS Nexus: Host–microbiome associations in saliva predict COVID-19 severity https://buff.ly/4aZ4fUi
The oral microbiome as a predictor of disease.
Integrated cytokine evaluations of saliva and serum showed that the oral host response was distinct from the systemic response.
“Our findings suggest that oral microbiome and salivary cytokines may be predictive of COVID-19 status and severity.”
4/18/24 Bloomberg: Covid Patient’s Infection Lasts 613 Days as Mutations Emerge https://buff.ly/3JmSlrE
A person with a blood disease that made him immunocompromised got an Omicron infection which became chronic for 20 months. During that time, the virus obtained over 50 mutations inside the man's body.
4/12/24 Nature: Signal Transduction and Targeted Therapy: Infection with SARS-CoV-2 can cause pancreatic impairment https://buff.ly/4aUmj24
SARS-CoV-2 infection in non-human primates (NHPs) and in people caused direct infection of both exocrine and endocrine pancreatic cells.
Increased insulin resistance, elevated fasting C-peptide and C-peptide/glucose ratio levels were noted after infection.
In older NHPs, SARS-CoV-2 infection caused loss of beta (β) cells, lower insulin production with islet amyloidosis and necrosis, and activation of α-SMA. There was also an increase of pancreatic inflammation and stress markers, ICAM-1 and G3BP1.
Vaccination maintained glucose homeostasis by activating insulin receptor α and insulin receptor β.
"Overall, the cumulative risk of diabetes post-COVID-19 is closely tied to age, suggesting more attention should be paid to blood sugar management in elderly COVID-19 patients."
4/10/24 PLOS Pathogens: SARS-CoV-2 infects cells lining the blood-retinal barrier and induces a hyperinflammatory immune response in the retina via systemic exposure https://buff.ly/3vRDBxS
4/7/24 Nature (Chendu, China): Systematic analyses of the factors influencing sperm quality in patients with SARS-CoV-2 infection https://buff.ly/3JkNs2f
Semen parameters were significantly reduced after SARS-CoV-2 infection, especially with fever. Semen gradually started to recover after 30 days post-infection, and exhibited no significant difference after 90 days compared with prior to COVID-19 infection.
Social, Advocacy and Disability
4/22/24 Charlie McCone has been denied SSDI again
https://twitter.com/loscharlos/status/1782498465244954749
Last week my SSDI was denied after waiting 16 months for decision. Lawyer said was most likely due to "independent Dr" @SocialSecurity sent me to in Feb who 1. Did not know what #LongCovid was 2. Refused to mask 3. Spent 10 minutes with me Has anyone had success on first appeal?
9:55 PM · Apr 22, 2024·41.9K Views
https://twitter.com/K_Bishof/status/1782527557440618782
Took me 2 denials & then a hearing to get approved. Having “residual functional capacity” forms completed by your clinicians for EACH condition you have is essential, as is finding an attorney who has been successful in arguing similar conditions. Highly recommend Nancy Cavey.
11:51 PM · Apr 22, 2024·1,002 Views
Seniors
4/15/24 Nature Microbiology: Age-specific nasal epithelial responses to SARS-CoV-2 infection https://buff.ly/3vVvi42
In kids (<12 years old), when nasal epithelial cells were infected with SARS-2, a distinct goblet inflammatory cell was seen, along with high expression of interferon-stimulated genes which stops viral replication.
In older adults (>70 years), nasal epithelial cells in culture that were infected with SARS-2 showed an increase in basaloid-like cells, which helped the virus spread.
ACE2 and TMPRSS2 receptors in nasal epithelial cells also differed between age groups.
4/17/24 Science Translational Med: Host-microbe multiomic profiling reveals age-dependent immune dysregulation associated with COVID-19 immunopathology https://buff.ly/3xEojwV
Older adults can be more susceptible to severe COVID infections. Using mass cytometry, serum proteomics, antibody assays, and transcriptional analysis, the authors found that older age was associated with increased viral load, reduced ability to clear the virus, and dysregulation of immune signaling. Older adults also had higher expression of pro-inflammatory genes and proteins with severe COVID infections.
There was also evidence of reactivation of herpes simplex and cytomegalovirus in older aged individuals in the upper airway.
Vaccines
4/16/24 BMC Infectious Diseases: Modelling the impact of hybrid immunity on future COVID-19 epidemic waves https://buff.ly/4d0Lh1y
"We find that if the past infection immunity is high but vaccination levels are low, then the secondary outbreak with the same variant can occur within a few months after the first outbreak; meanwhile, high vaccination levels can suppress near-term outbreaks and delay the second wave. Additionally, hybrid immunity has limited impact on future COVID-19 waves with immune-escape variants."
Immunity from prior COVID infection does not last very long and a second infection with the same variant can happen a few months after the first infection. But, vaccination can stop secondary infections with the same variant.
12/2022 Commonwealth Fund: Two Years of U.S. COVID-19 Vaccines Have Prevented Millions of Hospitalizations and Deaths https://buff.ly/3VThpeH
Antiviral treatments
4/16/24 Nature (Oxford, UK): Emerging variants develop total escape from potent monoclonal antibodies induced by BA.4/5 infection https://buff.ly/4cTCSgt
Twenty eight potent antibodies are isolated and characterised functionally, and in some cases structurally.
activity of some mAbs is regained on the recently reported variant BA.2.86.
Long COVID
6/2024 Current Problems in Cardiology: Attenuating post-exertional malaise in Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long-COVID: Is blood lactate monitoring the answer? https://buff.ly/3vDWW5E
"Lactate monitoring has the potential to extend beyond applied sports settings and could be used to monitor the physiologic and pathophysiological responses to external and internal stimuli in chronic disease areas such as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Post-Covid syndrome or Long Covid."
From ME Research UK:
https://twitter.com/MEResearchUK/status/1779872308452065313
Congrats to Prof. Akiko Iwasaki!
https://twitter.com/VirusesImmunity/status/1780575033770885152
Poorly done study in Nature magazine:
Study discussed that people with Long COVID have resolution of immune dysregulation at 24 months. But, their definition of Long COVID was if someone had “fatigue, dyspnea or chest pain.” They did not include people with cognitive dysfunction, post-exertional malaise, etc. They also lost more than 20% of their Long COVID patients to follow-up. In addition, some people with LC in the study were reinfected within the 24 months. They said that immune dysregulation resolved by 24 months in these people with fatigue, dyspnea or chest pain and then showed data that the people with Long COVID had EBV T cell exhaustion at 24 months. There are a lot of problems with this study.
4/17/24 Nature (Australia): Improvement of immune dysregulation in individuals with long COVID at 24-months following SARS-CoV-2 infection https://buff.ly/3U2j4yO
"These findings suggest resolution of immune activation in LC and return to comparable immune responses between LC and MC (matched recovered controls) over time.
Improvement in self-reported health-related quality of life at 24 months was also evident in the majority of LC (62%).”
Major problems with this study:
https://twitter.com/HarrySpoelstra/status/1780924321252131172
Study material: 2020, 90% of cases community-managed.
- 31 LC patients, 7 lost to follow-up at 24 months(=24 patients )
- 8 LC patients experienced a reinfection
- All participants in this sub-study were unvaccinated at acute infection and at enrolment, but most (85%) were subsequently fully vaccinated between 12- and 24-month , with no difference between the groups in terms of vaccine type
https://twitter.com/a_kruschke/status/1780952304323109166
The authors limited the inclusion to
"three major symptoms; fatigue, dyspnea, or chest pain".
Difference between control /LC in hospitalisation: 6% in control, 26% in LC group.
"T cell exhaustion scores calculated [..], no difference was observed between LC versus MC for any of the subsets analyzed .."
Hidden in the supplement: What about the EBV T-cell exhaustion?
4/12/24 Int J of Envir Research and Public Health: Pathophysiological Mechanisms in Long COVID: A Mixed Method Systematic Review https://buff.ly/43Y9b9X.
“The pathophysiological mechanisms with strong evidence were immune system dysregulation, cerebral hypoperfusion, and impaired gas transfer in the lungs.
“Other mechanisms with moderate to weak evidence were endothelial damage and hypercoagulation, mast cell activation, and auto-immunity to vascular receptors.
“Conclusions: LC is a complex condition affecting multiple organs with diverse clinical presentations (or traits) underpinned by multiple pathophysiological mechanisms. A ‘treatable trait’ approach may help identify certain groups and target specific interventions.”
Figure 3. Proposal causal network map for LC. Red for mechanisms well supported in this review and elsewhere, black for less strong evidence. Symptoms in green.
Jeremy Faust MD interviews NIH Director Monica Bertagnolli MD: U.S. 'Ready' for Next Pandemic Threat https://buff.ly/3xEQrQE
“Faust: I just want to follow up on something you said a moment ago about where this virus can be found in tissues. Are you suggesting that long COVID is actually, the mechanism of that persistent live virus in humans?
Bertagnolli: We see evidence of persistent live virus in humans in various tissue reservoirs, including surrounding nerves, the brain, the GI [gastrointestinal] tract, to the lung.
Faust: OK. And you're saying this goes beyond the PCR's [polymerase chain reaction test] ability to get it in a regular swab so that we are missing chronic cases of SARS‑CoV‑2?
Bertagnolli: Correct. The virus can persist in tissues for months, perhaps even years.
Faust: OK. I think that's certainly one theory, but I'm not sure that that's settled. Is that fair? I mean, there's one thing between people who are autopsy, they died of viral sepsis, as opposed to people walking around. Is there a distinction there?
Bertagnolli: Our emerging data shows that the virus can persist into tissues in the long term, and I think that's really critical because it does help us think about possible ways to combat it, one being better antivirals. I think there's a lot of focus on developing new antivirals as a possible way of preventing long COVID, and the other might be more aggressive treatment with antiviral therapy upon initial diagnosis.”
https://twitter.com/resiapretorius/status/1780675755627757788
4/9/24 NYAS: Long COVID and post-acute sequelae of SARS-CoV-2 pathogenesis and treatment: A Keystone Symposia report
Matthew S. Durstenfeld, Shannon Weiman, Michael Holtzman, Catherine Blish, Resia Pretorius, Steven G. Deeks https://buff.ly/3JizFsZ
In late summer of 2023, Keystone Symposia held the first scientific conference convening research leaders investigating the pathology behind Long COVID. The symposium “Long COVID and Post-Acute Sequelae of SARS-CoV-2 (PASC): Pathogenesis and Treatment” was held at the Eldorado Spa and Resort in Santa Fe, New Mexico August 27–30, 2023.
NeurologyLive® Friday 5 — April 12, 2024 https://buff.ly/3TZWxT2
Understanding Neurological Manifestations in Long COVID: Svetlana Blitshteyn, MD, FAAN
4/18/24 Neurology Today: Are Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Long COVID Part of the Same Disorder? A New NIH Initiative Aims to Find Out https://buff.ly/4aFJJIy
"Researchers say that exposure to an infection leads to concomitant and persistent immune dysfunction and changes in gut microbiome, which results in decreased concentrations of metabolites that then impact brain function."
“We believe these [ME/CFS and Long COVID] are virtually the same disease, although there are some differences, and they should be managed and studied in multidisciplinary clinics focused on post-infectious syndromes,” said lead author Avindra Nath, MD
Interviews with Dr. Avindra Nath, Dr. Hector Bonilla, Vicky Whittemore, PhD, Svetlana Blitshteyn, MD, Benjamin H. Natelson, MD
“Based on their data, ME/CFS is clearly a central nervous system disorder, and the associated fatigue is defined by autonomic dysfunction unrelated to psychological or psychiatric causes.” -Dr Blitshteyn
Dr. Nath's group has begun recruiting study participants for a clinical trial of intravenous IG (IVIG) in long COVID.
This study was discussed:
2/21/24 Nature: Deep phenotyping of post-infectious myalgic encephalomyelitis/chronic fatigue syndrome (PI-ME/CFS) https://buff.ly/3UNabLx
Small study: 17 people PI-ME/CFS vs. 21 healthy volunteers
PI-ME/CFS decreased functional status that was 1.5 to two standard deviations worse than the general population.The fatigue of PI-ME/CFS is due to decreased activity of the right temporal-parietal junction causing dysfunction of integrative brain regions that drive the motor cortex.
Dysregulation of catecholamine synthesis noted.
T cell exhaustion, seen by elevated PD-1 in cerebrospinal fluid (CSF).
Autonomic dysfunction with increase in sympathetic and a decrease in parasympathetic activity in PI-ME/CFS that affected HRV.
Sex differences in PI-ME/CFS in:
immune system responses including different gene expression in peripheral blood mononuclear cells (PBMCs)
muscles. Both males and females PI-ME/CFS samples had increased oxidative stress, but by different pathways.
CSF metabolites
PI-ME/CFS shows distinct sex differences in immune and metabolic dysregulation which suggest persistent antigenic stimulation.
Fig. 10: Pathophysiology of PI-ME/CFS
Exposure to an infection leads to immune dysfunction and changes in gut microbiome.
Immune dysfunction (from antigen persistence of pathogen) affects both innate and adaptive immune systems that are sex dependent.
These immune and microbial alterations impact the brain, leading to decreased concentrations of metabolites which impacts brain function.
The catecholamine nuclei release lower levels of catechols, which impacts the autonomic nervous system and manifests with decreased heart rate variability and decreased baroreflex cardiovascular function, with downstream effects on cardiopulmonary capacity.
Altered hypothalamic function leads to decreased activation of the temporoparietal junction during motor tasks, suggesting a failure of the integrative brain regions necessary to drive the motor cortex.
This decreased brain activity is experienced as physical and psychological symptoms and impacts effort preferences, leading to decreased engagement of the motor system and decreases in maintaining force output during motor tasks.
Both the autonomic and central motor dysfunction result in a reduction in physical activity. With time, the reduction in physical activity leads to muscular and cardiovascular deconditioning, and functional disability.
Summary from my past newsletter:
A new small study in Nature magazine looked at post-infectious myalgic encephalomyelitis/chronic fatigue syndrome (PI-ME/CFS). They found that fatigue in PI-ME/CFS is related to decreased activity of the right temporal-parietal junction in the brain. T cell exhaustion, as seen by elevated PD-1 in cerebrospinal fluid (CSF), dysregulation of catecholamine synthesis in the hypothalamus, and autonomic dysfunction with increase in sympathetic and a decrease in parasympathetic activity was found in people with PI-ME/CFS.
In addition, there were sex differences noted in PI-ME/CFS in immune system responses related to peripheral blood mononuclear cells (PBMCs) gene expression, increased oxidative stress noted in muscles via different pathways in men versus women, and sex differences in CSF metabolites. Their findings and possible mechanisms causing PI-ME/CFS, including Long COVID ME-CFS, are summarized in the figure below:
ME/CFS
https://twitter.com/OxMEDiscovery/status/1780304049104982368
Oct 13, 2023 U of Oxford: Diagnostic test can identify hallmarks of chronic fatigue syndrome in blood cells https://buff.ly/4aWG7Sf
Researchers at the University of Oxford led by Dr Karl Morten and Professor Wei Huang have developed the test, which has an accuracy rate of 91%
Funding needed.
8/31/23 Developing a Blood Cell‐Based Diagnostic Test for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Using Peripheral Blood Mononuclear Cells https://buff.ly/3Ur6KcH
Single-cell Raman platform and artificial intelligence were utilized to analyze blood cells.
Raman profiles of Peripheral Blood Mononuclear Cells (PBMCs) can distinguish between healthy individuals, disease controls, and ME/CFS patients with high accuracy (91%), and can further differentiate between mild, moderate, and severe ME/CFS patients (84%). Specific Raman peaks also correlate with ME/CFS phenotypes.
4/9/24 Neurology: Low Vasopressin in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) (P4-4.006) | Neurology https://buff.ly/4aOxl8S
Low vasopressin secretion in ME/CFS may underlie symptoms such as orthostatic intolerance.
4/9/24 Neurology: Actigraphic and Genetic Characterization of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Phenotypes in the UK Biobank (P10-9.007) | Neurology https://buff.ly/4aWeIA7
AI:
4/17/24 Science Translational Medicine: Deep learning assists detection of esophageal cancer and precursor lesions in a prospective, randomized controlled study https://buff.ly/4aH9kBc
Eric Topol MD: “In a randomized controlled trial, machine vision #AI during endoscopy doubled the detection rate of esophageal cancer and precursor lesions.”
Other news:
4/22/24 PNAS (Yale): Intranasal neomycin evokes broad-spectrum antiviral immunity in the upper respiratory tract https://buff.ly/3W6ihPZ
Neosporin ointment placed in the nose may help prevent COVID and the flu. Intranasal generic antibiotic neomycin increased interferon expression in the nose and protected mice and hamsters from COVID infection and from Influenza A. In humans, Neosporin also increased interferon expression in the nose.
4/10/24 Science: Noninvasive virtual biopsy using micro-registered optical coherence tomography (OCT) in human subjects https://buff.ly/3U8zCVX
“We’ve not only created something that can replace the current gold-standard pathology slides for diagnosing many conditions, but we actually improved the resolution of these scans so much that we start to pick up information that would be extremely hard to see otherwise,” said Adam de la Zerda, PhD
4/2024 ACOG: Screening for Syphilis in Pregnancy https://buff.ly/3UpDtz2
Because of “rapidly increasing rates of congenital syphilis, obstetrician–gynecologists and other obstetric care professionals should screen all pregnant individuals serologically for syphilis at the first prenatal care visit, followed by universal rescreening during the third trimester and at birth, rather than use a risk-based approach to testing.”
4/16/24 Nature Medicine: Placental IGFBP1 levels during early pregnancy and the risk of insulin resistance and gestational diabetes https://buff.ly/4498laj
Transcriptomic profiling of 434 human placentas and identified a positive association between insulin-like growth factor binding protein 1 gene (IGFBP1) expression in the placenta and insulin sensitivity at ~26 weeks gestation.
a role for placental IGFBP1 deficiency in GDM pathogenesis.
A deficit in the way the placenta expresses the gene for a hormone called insulin-like growth factor 1 (IGF-1) appears linked to insulin resistance during pregnancy,
4/2/24 Short-chain fatty acids: linking diet, the microbiome and immunity - Nature Reviews Immunology https://buff.ly/3VX1gYc
Fig. 1: Environmental factors drive microbial metabolism and diversity with effects on short-chain fatty acid production and inflammation.
a, Environmental and host factors including birth mode, breastfeeding, diet, genetics, biological sex, age, use of antibiotics and inflammation modify the composition and metabolic capacity of intestinal microbial communities.
Many of these factors have been shown to affect butyrogenic bacterial communities, such as Faecalibacterium prausnitzii, Anaerostipes spp., Roseburia spp. and Eubacterium spp., and the levels of butyrate in the intestine, as well as production of other short-chain fatty acids (SCFAs) including acetate and propionate.
Cross-feeding between butyrate-producing and non-producing strains contributes to the production of butyrate.
4/3/24 NEJM: Trial of Lixisenatide (GLP-1) in Early Parkinson’s Disease https://buff.ly/4aFCqAL
4/15/24 Nature: Prasinezumab slows motor progression in rapidly progressing early-stage Parkinson’s disease https://buff.ly/3TY2HTF
Prasinezumab is a monoclonal antibody that binds aggregated α-synuclein




























Another great update - thank you.
Thank you! As always, great content! I look forward to your newsletter each weekend and was worried (that maybe you got Covid) when it didn't appear on Saturday or Sunday. Enjoy your vacation!