We continue to be at “LOW” levels of COVID now in the U.S. according to wastewater levels of SARS-CoV-2. There are no states at the “HIGH” level this week which is good news. Hospitalizations, Emergency Department visits and deaths from COVID continue to decrease significantly. JN.1 and its progeny continue to make up almost all cases of COVID. According to JP Weiland, we are still at relatively low levels of SARS-CoV-2 transmission and approximately every 1 in 142 people is currently infected.
At times, it has been hard for some people to access Paxlovid for an acute COVID infection. That is why it was very helpful to have the Test to Treat program where a person who tested positive for either the flu or COVID could get free telehealth visits and free medications (Tamiflu for the flu, Paxlovid for COVID). The program which was supported by the NIH and the ASPR will be ending next Tuesday April 16, 2024, Dr. Judy Stone reported on Forbes. Regarding testing, a new over-the-counter test has been approved by the FDA from CorDx which will allow people to test at home for Influenza A, Influenza B and SARS-CoV-2 all in one multiplex test.
Nanobodies from camels are smaller neutralizing antibodies that are easier to produce than conventional monoclonal antibodies and they have low immunogenicity. A group from Beijing immunized a camel with the SARS-CoV-2 spike protein. The camel produced two nanobodies (C-282 and C-39) with broad neutralizing activity against pre-Omicron variants and five Omicron variants (BA.1–5).
From: https://pubmed.ncbi.nlm.nih.gov/38603467/
Regarding acute COVID infections, a group from Stanford discovered that a special type of macrophage cell in the lungs called interstitial macrophages are responsible for the transition from a moderate COVID infection to a life threatening COVID infection associated with ARDS (Acute Respiratory Distress Syndrome). Macrophages are a type of white blood cell that surrounds and kills bacteria and viruses. They also remove dead cells in the body and they stimulate other immune system cells as needed.
In the lungs, there are two types of macrophages- alveolar macrophages (AM) that reside within the alveoli in the area where oxygen and carbon dioxide are exchanged and interstitial macrophages (IM) that live in the interstitial area between the endothelial cells of tiny blood vessels in the lungs and the cells that line the alveoli. The SARS-CoV-2 virus enters most cells in the human body via the ACE2 receptor, but the virus infects interstitial macrophages via a different cell receptor called CD209. This study showed that IMs are the main site of viral infection deep in the lungs which can lead to inflammation and fibrosis of the architecture of lung tissues. Blocking the CD209 receptor may decrease the risk of severe COVID infection and ARDS.
Looking at the entire population of Norway (5.4 million people), a new study shows that COVID vaccination reduced the risk of Long COVID by about 40%. COVID vaccination also reduced post-COVID thrombotic and cardiovascular complications (heart failure, venous blood clots, arterial blood clots) by 40 to 50%.
Long COVID incidence
238,828 U.S. blood donors, of which 83,015 had a history of COVID infection, were surveyed in 2022. The most commonly reported long-term symptoms were difficulty thinking and fatigue. Prior COVID infection was associated with 2.5-fold increased risk of long-term symptoms, as compared to people who did not have a history of prior COVID infection. A KFF article shows that 1 in 10 people have Long COVID now and that 79% of them have limitations on their activities because of Long COVID.
Viral persistence of the SARS-CoV-2 virus somewhere in the body has been thought to be a cause of Long COVID. A new study from UCSF and Harvard shows that 25% of people tested showed viral persistence of SARS-CoV-2 proteins (spike, S1 or N proteins) in their blood up to 14 months after COVID infection. The risk of viral persistence was two-times more common in people who had been hospitalized with their acute COVID infection. This week, there was a well-written article in Science Magazine looking at ongoing clinical studies of medications and treatments for viral persistence of SARS-CoV-2 virus in Long COVID. Medications being tested for viral persistence in Long COVID include Paxlovid, the monoclonal antibody AER002, Larazotide (reduces gut permeability in Celiac Disease), SARS-2 antiviral Ensitrelvir and a trial of Truvada with Selzentry (Maraviroc) which are two HIV antiviral drugs.
From: https://www.science.org/content/article/long-covid-trials-aim-clear-lingering-virus-help-patients-need
This week, Bernie Sanders released a draft for a proposed “Long COVID Moonshot” bill giving $1 Billion per year for 10 years to Long COVID research. Bernie is asking for input from people with Long COVID, their caregivers and from healthcare professionals here. “Please submit your comments to the Committee by email at LongCOVIDComments@help.senate.gov no later than the close of business on Tuesday, April 23, 2024.”
Fibrinaloid Microclots and Long COVID
This week, there were two articles about fibrinaloid microclots in Long COVID. Normally, when someone gets a cut, platelets go to the area and form a soft plug. The coagulation cascade is then triggered with one coagulation factor being converted to the next until fibrinogen is made into fibrin. Fibrin makes a sort of net around platelets and red blood cells to make the clot more stable and strong.
Amyloid refers to a type of protein that is formed in a beta-sheet pattern. While fibrinogen is a normal part of the blood clotting cascade, in Long COVID, fibrinogen can group together or polymerize into atypical blood clots containing amyloid that are called fibrinaloid microclots. Fibrinaloid microclots are resistant to normal fibrinolysis in the body. Natto is a fermented food made of soybeans that is eaten in Japan and is touted to have health benefits. Nattokinase is made from natto and is a protease enzyme with fibrinolytic activity that can break down typical blood clots that do not contain amyloid. This new study shows that in vitro, nattokinase can break down fibrinaloid microclots found in Long COVID. The article also describes an automated way to count fibrinaloid microclots in the blood using a fluorescent dye. The authors concluded that the formation kinetics of fibrin amyloid microclots in the blood can be imaged noninvasively in an automated manner using the fluorogenic stain thioflavin T, that these microclots were found to aggregate over time, and that these fibrinaloid microclots can be degraded by nattokinase.
Another group from Sheffield in the UK, used the same fluorescent dye Thioflavin T (ThT) to measure fibrinaloid microclots from platelet-poor plasma. They found that there were elevated numbers of fibrinaloid microclots in both Long COVID and acute COVID infection as compared to controls. In acute COVID infections however, the number of fibrinaloid microclots decreased over time. They also found higher levels of fibrinaloid microclots in females with Long COVID as compared to males with Long COVID and to healthy volunteers of both sexes.
Figure 2 – Microclot counts from PPP samples.
UC – Uninfected Controls (individuals who have not knowingly been exposed to COVID),
CC – COVID Controls (had a positive COVID lateral flow or PCR test in the past),
LC – Long COVID (persistent symptoms at least three months after a COVID infection).
RC – Recent COVID (positive COVID test within the previous three weeks).
Figure 3– Microclot counts from PPP samples split by sex. CF – Control female, LCF – Long COVID female, CM – Control male, LCM – Long COVID male.
From: https://www.medrxiv.org/content/10.1101/2024.04.04.24305318v1
Mitochondrial dysfunction in Long COVID
Mitochondria are called the powerhouse of the cell as they make energy. By using multiplatform metabolomics analysis (CE-MS, GC-MS, and LC-MS), a new study found more evidence of mitochondrial dysfunction in Long COVID. Forty-six metabolites were different between people with Long COVID and fully recovered patients. Specific abnormal metabolites in Long COVID showed a decrease in the amino acid metabolism and ceramide plasma levels and an increase in the tricarboxylic acid (TCA) cycle, all which point to mitochondria not working normally. They also found elevated cytokine plasma levels of IL-6 and TNF-α in Long COVID which may lead to activation of proinflammatory macrophages.
Figure 7. Interconnections between the metabolic pathways of the relevant dysregulated metabolites. Green-squared and red-squared metabolites indicate increased and decreased levels, respectively, in Long COVID when compared to individuals fully recovered from acute COVID-19.
From: https://pubs.acs.org/doi/abs/10.1021/acs.jproteome.3c00706
Neuro Long COVID and Cognitive Dysfunction
Dani Beckman PhD is a neuroscientist specialized in high-resolution microscopy who works at the California National Primate Center. She posted on Twitter about two different papers this week on neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP) as blood biomarkers for Neuro Long COVID. The first study in Nature magazine showed that at ten months after resolution of mild or even asymptomatic SARS-CoV-2 infection, people with cognitive impairment had elevated serum levels of NFL and/or GFAP. Elevated NFL in the blood means that there is ongoing damage to the axons of nerves in the brain (or spinal cord). Glial fibrillary acidic protein (sGFAP) in the blood means that there is abnormal activation of astrocytes in the brain. Although levels of serum NFL and GFAP decreased over time in people with Neuro Long COVID cognitive symptoms, they still remained higher than those of the controls who had not had a prior COVID infection. This suggests ongoing brain damage to both neurons and astrocytes in Neuro Long COVID.
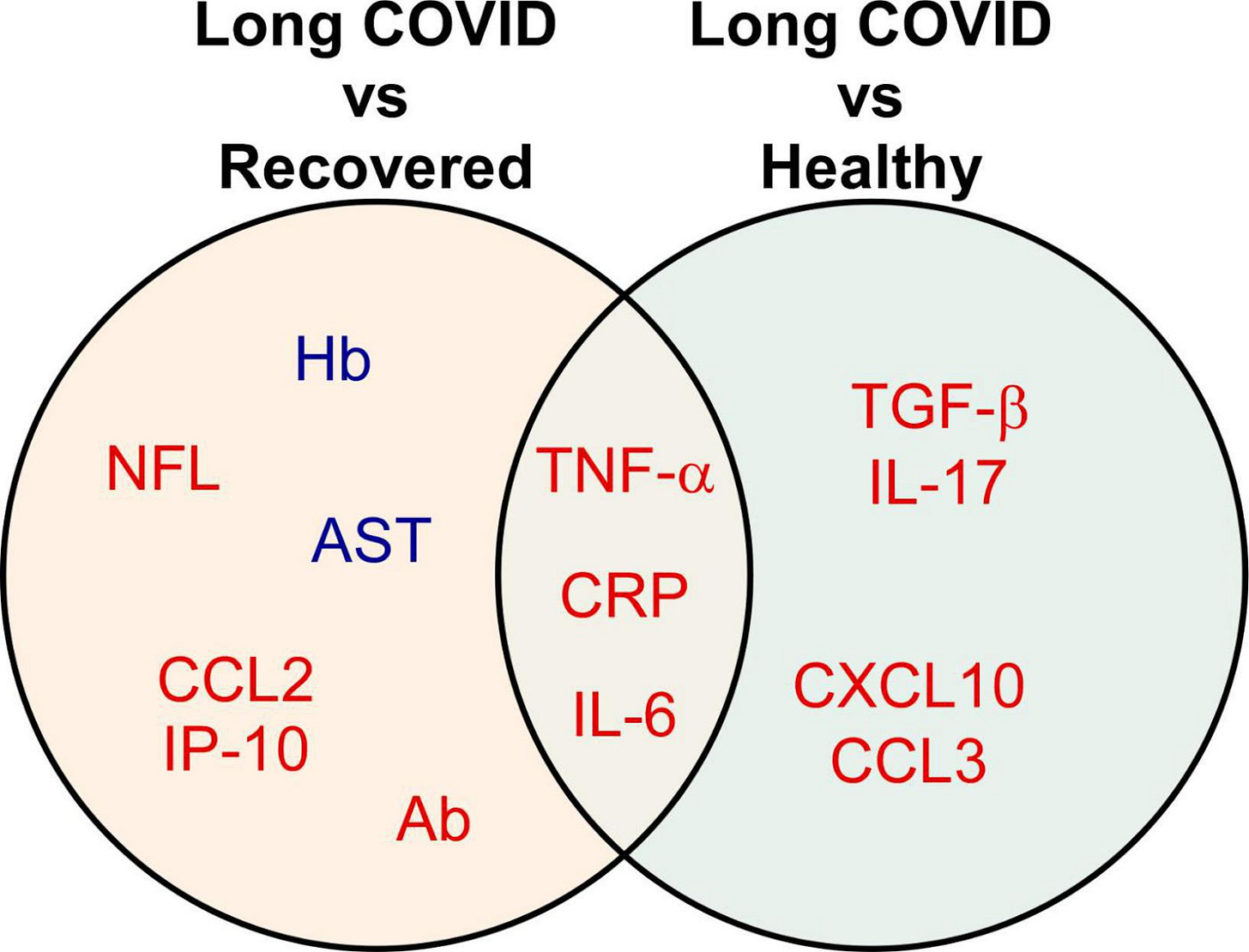
A second study on Neuro Long COVID biomarkers that Dr. Beckman referred to was from January 2023. This review showed that IL-6, CRP, and TNF-alpha can be used as biomarkers for Long COVID, neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP) are biomarkers for Neuro Long COVID and cognitive impairment, and that elevated TGF-beta is related to pulmonary symptoms in Long COVID.
Figure 3. Biomarkers significantly associated with different comparison groups. The Venn diagram presents the 13 biomarkers that were reported by two or more eligible studies.
Red indicates up-regulated, while blue refers to down-regulated biomarkers.
Figure 4. Biomarkers of long COVID symptoms. The Venn diagram presents the 41 biomarkers that were reported by two or more eligible studies. Red indicates up-regulated, while blue refers to down-regulated biomarkers.
From: https://www.frontiersin.org/articles/10.3389/fmed.2023.1085988/full#main-content
Cardiac findings after COVID infection
A group in Italy registered patients in a non-randomized fashion when they had a positive SARS-CoV-2 test and followed them until their test was negative. They then did lab tests and cardiac testing (ECG, Holter, and TTE) about 5 months after their negative COVID test and found new cardiac abnormalities in 9.6% to 42.5% of them depending on whether patients had been hospitalized or not with their acute COVID infection and if they had post-acute COVID symptoms. At 5.5 months, 68% were still symptomatic whether or not they had been hospitalized with their acute COVID infection. The most common post-acute symptoms were shortness of breath, weakness, heart palpitations, fatigue and anxiety or depression.
At more than 5 months after COVID infection, cardiac abnormalities were found in:
9.6% of people who had Mild COVID, with no post-acute symptoms.
23% of people who had Mild COVID, that did have post-acute symptoms.
28% of people who had been Hospitalized for COVID, with no post-acute symptoms.
42.5% of people who had been Hospitalized for COVID, that did have post-acute symptoms.
Overall, 27% of patients had new cardiac abnormalities as seen on ECG, Holter monitor and TTE. Pericardial effusion was especially common at 12% of patients. If a patient has been hospitalized for their acute COVID infection, or if they have post-acute COVID symptoms, the authors recommend that these patients undergo cardiac testing.
Dr. Svetlana Blitshteyn relayed an important case on Twitter about a 49 year old man who had a heart attack. The EHR (medical records) did not mention that the man had a COVID infection 12 weeks before his heart attack. Dr. Blitshteyn reminds us that “cardiovascular, autonomic and neurologic manifestations of COVID are widespread and are often not recognized or coded as such, and therefore will not be tracked in the electronic medical records. People are having heart attacks, strokes and blood clots at a young age, which are not counted as post-Covid sequelae, thus, the real incidence and prevalence of Long Covid and post-Covid conditions are largely underestimated. Patients are not started on aspirin [after heart attack] because "there is no blockage in the arteries," but many patients are in hypercoagulable state (his d-dimer on admission was high), therefore at least a daily aspirin might be beneficial. Long COVID is a major public health issue that is under-reported, under-counted, under-recognized and under-treated.”
Post Hospitalization, Long COVID subtypes
A group from the Imperial College London did proteome studies of people who had Long COVID symptoms after being hospitalized with COVID. They found that elevated markers of myeloid inflammation and complement activation were associated with Long COVID. Specific proteins were increased in different Long COVID subtypes related to symptoms. The authors postulated that common pathways causing Long COVID symptoms could be targeted with certain medications. “Our finding of increased sCD58 levels (associated with suppression of monocyte–lymphocyte interactions) in the recovered group, strengthens our conclusion that myeloid inflammation is central to the biology of LC and that trials of steroids, IL-1 antagonists, JAK inhibitors, naltrexone and colchicine are justified.” They also recommended considering the judicious use of anticoagulants and antiviral medications (singly or a combination of antivirals) to treat Long COVID.
Figure 10: Graphical Abstract https://www.nature.com/articles/s41590-024-01778-0/figures/14
Long term sequelae of COVID infection in Multiple Sclerosis patients
Compared to Multiple Sclerosis patients without COVID-19, Multiple Sclerosis patients who had a COVID-19 infection early in the pandemic were found to have 4x increased mortality risk, 3x increased post infection optic neuritis, >4x need for methylprednisolone treatment for MS relapse and a higher risk of hospitalization (78.92% vs. 66.81%, p<0.01). “MS patients who survived COVID-19 infection experienced worse long-term outcomes, as measured by treatment for relapse, hospitalization and mortality. Identifying risk factors for worse long-term outcomes may draw clinical attention to the need for careful follow-up of at-risk individuals post-SARS-CoV-2 infection.”
ME/CFS
Whitney Dafoe is a person with severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) whose data has been followed longitudinally over many years by his father, Stanford researcher Ron Davis. This week, they published longitudinal cytokine and multi-modal health data with several important summary diagrams. They found that dysregulated Th2-type cytokines could be helpful for “patient stratification and precision medicine strategies.” Figure 3 details severity levels of ME/CFS and Figure 7 summarizes potential mechanisms underlying ME/CFS with possible biomarkers and therapeutic targets. “The synergistic activity of mast cells and eosinophils upon systemic activation can skew Th1/Th2 to Th2-immune responses, leading to tissue injuries, autoimmunity, impairment of multiple organs and biological systems as well as causing exercise intolerance and post-exertional malaise in predisposed individuals. Unresolved systemic mast cell and eosinophil overactivation could contribute to the development and aggravation of ME/CFS and related multisystem disorders and comorbidities.”
Figure 7 summarizes how Mast Cells, Eosinophils and T helper cell abnormalities can lead to ME/CFS:
From: https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1369295/full
In non-COVID news, The National Academy of Medicine presented a draft of an artificial intelligence (AI) code of conduct principles for health care and biomedical science. A rare genetic variation in fibronectin 1 (FN1) was found to protect against APOEε4 mutations in Alzheimer’s disease risk. Massachusetts General Hospital confirmed that their first patient to receive a genetically modified pig kidney transplant is doing well and was discharged from the hospital.
Human touch is beneficial to both our physical and mental health as seen by a new review. Ozempic and other GLP-1 medications may cause some women to become more fertile. Decreasing body fat can cause some women, such as women with PCOS, to ovulate. It is also unknown if birth control pills are as effective with GLP-1 medications.
A total solar eclipse was seen across many places in the United States last week. The moon tweeted a witty quip, and Airbnb rentals were fully booked along the path of the eclipse. Anirban Maitra posted a picture of a welcome kit from his Airbnb host which included Eclipse gum, Starry soda, Sun chips and Moon Pies, as well as eclipse glasses.
Have a good rest of your weekend,
Ruth Ann Crystal MD
_________________
COVID news notes:
US Variant tracker: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
Variants around the world: https://outbreak.info/
World wastewater maps (reflects COVID cases): https://www.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082
CDC COVID data tracker: https://covid.cdc.gov/covid-data-tracker/index.html#datatracker-home
Test positivity 3.5%
ED visits down -14.5%
Hospitalizations down -15.3%
Deaths down -20%
CDC COVID Hospitalizations (blue) and Emergency Room (orange) visits tracker: https://covid.cdc.gov/covid-data-tracker/index.html#trends_weeklyhospitaladmissions_7dayeddiagnosed_00
Walgreens positivity rate: https://www.walgreens.com/businesssolutions/covid-19-index.jsp
US Wastewater Monitoring:
CDC wastewater reporting: https://www.cdc.gov/nwss/rv/COVID19-nationaltrend.html
CDC wastewater map: https://www.cdc.gov/nwss/rv/COVID19-currentlevels.html
Biobot: https://biobot.io/data/
National SARS-CoV-2 data from Sara Anne Willette: https://iowacovid19tracker.org/
There are no states in the substantial, high or excessively high categories now.
Wastewater SCAN: https://data.wastewaterscan.org/
California statewide view https://buff.ly/3YObiul
Sewer Coronavirus Alert Network (SCAN) project by Stanford University:
Santa Clara County wastewater: https://covid19.sccgov.org/dashboard-wastewater
Marin county: https://coronavirus.marinhhs.org/surveillance
CDC Respiratory vaccination trends: https://www.cdc.gov/respiratory-viruses/data-research/dashboard/vaccination-trends-adults.html
JP Weiland: https://twitter.com/JPWeiland
https://twitter.com/JPWeiland/status/1779562832440295506
April 14th Update:
Modest declines this week, still at relatively low levels of transmission. All regions roughly similar, South is slightly higher:
235,000 new infections/day
~2.77 avg total infections per capita across the US
1 in every 142 people currently infected
Michael Hoerger modeling: http://pmc19.com/data/, https://twitter.com/michael_hoerger
Acute COVID infections, General COVID info
4/10/24 Interstitial macrophages are a focus of viral takeover and inflammation in COVID-19 initiation in human lung | Journal of Experimental Medicine | Rockefeller University Press (Irv Weissman, Stephen Quake, Catherine Blish, Mark Krasnow) https://buff.ly/49A5CIa
A new study finds that a previously overlooked type of immune cell, interstitial macrophage is the most susceptible cell to infection by SARS-CoV-2 that’s responsible for the critical transition from a merely bothersome COVID-19 case to a potentially deadly one!
What’s more, the virus enters this susceptible cell via an unexpected route. SARS-CoV-2 was not using ACE2 to get into interstitial macrophages. It enters via another receptor called CD209.
Interstitial macrophages (IM) are situated deep in the lungs, protecting it by viruses, bacteria, fungi & dust particles that make their way down our airways. But it’s these very cells, that of all known types of cells of lung tissue are most susceptible to infection by SARS2
4/8/24 Dr Judy Stone for Forbes: Important Program For Covid Patients Closes, Leaving Many Stranded https://buff.ly/4awJ6kK
The home “Test to Treat” program is closing April 16. It allowed people to test for flu and COVID and get antivirals without health insurance.
Antiviral treatments
4/11/24 J of Proteome Research from ACS: Proteomics Platform Reveals Broad-Spectrum Nanobodies for SARS-CoV-2 Variant Neutralization https://buff.ly/3xygYiy
They immunized a camel with SARS-CoV-2 spike protein. The camel produced two nanobodies (C-282 and C-39) with broad neutralizing activity against pre-Omicron variants and five Omicron variants (BA.1–5).
Nanobodies from camels are smaller neutralizing antibodies that are easier to produce and have low immunogenicity.
COVID testing
https://twitter.com/michaelmina_lab/status/1778182342445834674
Long COVID
4/11/24 Science: Long Covid trials aim to clear lingering virus—and help patients in need https://buff.ly/3xvMbmq
Great article looking at different studies of medications and treatments of possible viral persistence of SARS-CoV-2 virus in Long COVID.
Ongoing clinical trials for viral persistence in Long COVID including Paxlovid, monoclonal antibody AER002, Larazotide (reduces gut permeability in Celiac Disease), Ensitrelvir antiviral and a trial of Truvada with Selzentry (Maraviroc) which are two HIV antiviral drugs.
4/10/24 Lancet Respiratory: Effectiveness of COVID-19 vaccines to prevent long COVID: data from Norway https://buff.ly/3TWDucd
Looking at the entire population of Norway (5.4 million people), COVID vaccination reduced the risk of Long COVID by about 40%.
COVID vaccination also reduced post-COVID thrombotic and cardiovascular complications (heart failure, venous blood clots, arterial blood clots) by 40 to 50%.
A group surveyed 238,828 blood donors in 2022, of which 83,015 had a history of COVID infection. Difficulty thinking and fatigue were the most commonly reported symptoms. Prior COVID infection was associated with 2.5-fold increased risk of long term symptoms, as compared to people who did not have a history of prior COVID infection.
4/9/24 CIDRAP: Blood donor study in JAMA finds 21% incidence of long-term symptoms attributed to COVID-19 https://buff.ly/4438T1y
Of the 83,015 people with a history of SARS-CoV-2 infection, 43.3% reported new long-term symptoms compared with 22.1% of those without a history of SARS-CoV-2 infection (adjusted odds ratio [AOR], 2.55; 95% confidence interval [CI], 2.51 to 2.61).
Being a woman and having history of chronic health conditions was associated with long COVID symptoms.
Among blood donors with prior SARS-CoV-2 infection,
23.6% neurologic symptoms,
23.1% reported other symptoms (including changes in taste or smell),
15.8% reported respiratory or cardiac symptoms,
11.9% reported mental health symptoms, and
4.6% reported gastrointestinal symptoms
Difficulty thinking, fatigue most common symptoms after COVID infection.
4/8/24 JAMA: Long-Term Symptoms Associated With SARS-CoV-2 Infection Among Blood Donors https://buff.ly/3Udowjr
238,828 survey participants, 43.3% of those with a history of SARS-CoV-2 infection reported new long-term symptoms compared with 22.1% without a history of infection.
Long-term symptoms lasting more than 4 weeks are common in the adult population, but there is a significantly higher prevalence among those with SARS-CoV-2 infection.
4/2/24 Journal of Proteome Research from ACS: Reinforcing the Evidence of Mitochondrial Dysfunction in Long COVID Patients Using a Multiplatform Mass Spectrometry-Based Metabolomics Approach https://buff.ly/3UoxJG1
a multiplatform mass spectrometry-based approach was used for metabolomic and lipidomic profiling of human plasma samples from Long COVID patients (n = 40) to reveal mitochondrial dysfunction when compared with individuals fully recovered from acute mild COVID-19 (n = 40).
46 metabolites were different between Long COVID and fully recovered patients.
Specific metabolites altered in Long COVID, mainly related to a decrease in the amino acid metabolism and ceramide plasma levels and an increase in the tricarboxylic acid (TCA) cycle, reinforcing the evidence of an impaired mitochondrial function.
Graphic Abstract:
Figure 7. Interconnections between the metabolic pathways of the relevant dysregulated metabolites. Green-squared and red-squared metabolites indicate increased and decreased levels, respectively, in Long COVID when compared to individuals fully recovered from acute COVID-19.
4/9/24 Chairman Bernie Sanders Releases Long COVID Moonshot Legislative Proposal https://buff.ly/3Q1AE4D
Sen. Bernie Sanders (I-Vt.), Chair of the Senate Health, Education, Labor, and Pensions (HELP) Committee, released a draft legislative proposal to address the Long COVID crisis that is negatively impacting the health of some 22 million Americans.
Bernie Sanders released a draft for proposed Long COVID Moonshot legislation, which would earmark $1 billion per year over 10 years for Long COVID research.
https://twitter.com/zalaly/status/1777814888393355591
https://twitter.com/tmprowell/status/1778836248938901857
Bernie Sander’s letter to Long COVID Stakeholders: https://www.sanders.senate.gov/wp-content/uploads/4.9.2024-Factsheet_The-Long-COVID-Moonshot-Act.pdf
“We invite your input on the more detailed proposal (HERE). Please submit your comments to the Committee by email at LongCOVIDComments@help.senate.gov no later than the close of business on Tuesday, April 23, 2024.”
4/5/24 Pre-print in International Journal of Cardiology Cardiovascular Risk and Prevention (Italy): High prevalence of Cardiac post-acute sequelae in patients recovered from Covid-19. Results from the ARCA post-COVID study https://buff.ly/3U9GrHY
Multisite observational study in Italy. No control group.
From June 2020 to December 2022, 502 patients with a positive nasopharyngeal swab for SARS-CoV2 were enrolled. Demographics included 52% women, 76% mild COVID cases.
Lab tests and cardiac evaluation (ECG, Holter, TTE) were performed a median of 76 days after patients tested negative for COVID.
Conclusion
A group in Italy registered patients when they had a positive SARS-CoV-2 test and followed them until their test was negative. They did lab tests and cardiac testing about 76 days after their negative COVID test and found new cardiac abnormalities in 9.6% to 42.5% of them depending on whether patients had been hospitalized or not with their acute COVID infection and if they had post-acute COVID symptoms. More than 6 months after the SARS-CoV2 infection, 77% of patients were still symptomatic, regardless of hospitalization or home treatment.The most common post-acute symptoms were shortness of breath, weakness, heart palpitations, fatigue and anxiety or depression.
Post-acute cardiac abnormalities were found in:
9.6% had abnormal cardiac findings for Mild COVID, with no post-acute symptoms.
23.3% had abnormal cardiac findings for Mild COVID, that had post-acute symptoms.
28% had abnormal cardiac findings for patients Hospitalized for COVID, with no post-acute symptoms.
42.5% had abnormal cardiac findings for patients Hospitalized for COVID, that had post-acute symptoms.
If a patient has been hospitalized for their acute COVID infection, or if they have post-acute COVID symptoms, the authors recommend that these patients undergo cardiac testing.
If 9.6% of patients with mild initial COVID infections and no post-acute symptoms were found to have cardiac abnormalities, who should we be screening?
We should at least screen people who had mild COVID and have some post-acute symptoms because 23% of them were found to have cardiac abnormalities at 6 months post COVID infection.
That means that a lot of people should probably be tested 6 months after COVID with cardiac screening.
Figure 2. Prevalence of abnormal cardiac findings based on symptoms and prior hospitalization for COVID.
A: Mild COVID, no post-acute symptoms (9.6% had abnormal cardiac findings)
B: Mild COVID, with post-acute symptoms (23.3% had abnormal cardiac findings)
C: Hospitalized for COVID, no post-acute symptoms (28% had abnormal cardiac findings)
D: Hospitalized for COVID, with post-acute symptoms (42.5% had abnormal cardiac findings)
----
A group from the Imperial College London did proteome studies of people who had Long COVID symptoms after being hospitalized with COVID. They found that elevated markers of myeloid inflammation and complement activation were associated with Long COVID. Specific proteins were increased in different Long COVID subtypes related to symptoms. The authors ____ that there are some common pathways causing Long COVID symptoms that could be targeted with certain medications. “Our finding of increased sCD58 levels (associated with suppression of monocyte–lymphocyte interactions) in the recovered group, strengthens our conclusion that myeloid inflammation is central to the biology of LC and that trials of steroids, IL-1 antagonists, JAK inhibitors, naltrexone and colchicine are justified.” They also recommended considering the judicious use of anticoagulants and antiviral medications (singly or a combination of antivirals) to treat Long COVID.
4/8/24 Nature Immunology: Large-scale phenotyping of patients with long COVID post-hospitalization reveals mechanistic subtypes of disease https://buff.ly/3xr9gqm
657 participants ≥3 months following hospitalization for acute COVID infection
"Our study aimed to understand inflammatory processes that underlie long COVID and was not designed for biomarker discovery."
Elevated markers of myeloid inflammation and complement activation were associated with Long COVID.
Severe acute respiratory syndrome coronavirus 2-specific immunoglobulin G (IgG) was persistently elevated in some individuals with long COVID, but virus was not detected in sputum.
Figure 10: Graphical Abstract https://www.nature.com/articles/s41590-024-01778-0/figures/14
4/8/24 PolyBio Research Fd: COVID-19 Virus Can Persist in the Body More Than a Year after Infection https://buff.ly/49sfIKV
"The researchers [Peluso et al, study below] analyzed blood samples from 171 people who had been infected with the virus. Using a novel ultra-sensitive blood test, they found that proteins from the virus were still present up to one year after infection in up to 25% of people. These findings greatly bolster evidence that the coronavirus can linger in tissue and organs, even after recovery from acute infection.
The likelihood of detecting the COVID proteins indicative of persistent virus was about twice as high among those who were hospitalized for COVID as it was for those who were not. It was also higher for those who were not hospitalized but reported being sicker. "
4/8/24 Lancet: Peluso et al: Plasma-based antigen persistence in the post-acute phase of COVID-19 https://buff.ly/3U7lnBR
This study shows viral persistence of SARS-CoV-2 antigens in blood samples up to 14 months after an acute COVID infection. The risk of persistence was two-times more common in people who had been hospitalized with their acute COVID infection.
“Of 660 pandemic-era specimens tested, 61 (9·2%) specimens from 42 participants (25% of the group), had one or more detectable SARS-CoV-2 antigens.”
“Our data provide strong evidence that SARS-CoV-2, in some form or location, persists for up to 14 months following acute SARS-CoV-2 infection.
25% of samples from the pandemic era showed viral persistence of SARS-CoV-2 antigens (spike, S1 or N proteins).
Patients who had been hospitalized were almost twice as likely to have persistent viral antigens in their blood than people who had not been hospitalized.
Figure B: The absolute difference in SARS-CoV-2 plasma antigen prevalence:
10.6% at 3 to 6 months after acute COVID infection
8.7% from 3 to 10 months after acute COVID infection
5.4% at 10 to 14 months after acute COVID infection
Preprint of this study:
10/26/23 MedRxiV (UCSF, Harvard): Plasma-based antigen persistence in the post-acute phase of SARS-CoV-2 (PACS) infection https://buff.ly/3rZcaQZ
Fibrinaloid Microclots and Long COVID
4/7/24 BioRxiV (Preprint of the International Journal of Molecular Science- Resia Pretorius and Doug Kell): Automated microscopic measurement of fibrinaloid microclots and their degradation by nattokinase, the main natto protease https://buff.ly/3TWxBfl
Normally, when someone gets a cut, platelets go to the area and form a soft plug. The coagulation cascade is triggered with one coagulation factor being converted to the next until fibrinogen is made into fibrin. Fibrin makes a sort of net around platelets and red blood cells to make the clot more stable and strong.
Fibrinogen promotes platelet aggregation by stimulating platelet clumping.
Amyloid is a type of protein that is formed by beta-sheets of certain peptides. While fibrinogen is a normal part of the blood clotting cascade, in Long COVID, fibrinogen can polymerize into atypical blood clots containing amyloid called fibrinaloid microclots that are resistant to normal fibrinolysis in the body. Natto is a fermented food made of soybeans that is eaten in Japan and is touted to have health benefits. Nattokinase is made from natto and is a protease enzyme with fibrinolytic activity that can break down typical blood clots that do not contain amyloid. This study shows that in vitro, nattokinase can help break down fibrinaloid microclots found in Long COVID and therefore may be a helpful treatment for some of Long COVID’s symptoms.
conclude at least three important features:
(i) the formation kinetics of fibrin amyloid microclots in whole samples may be imaged noninvasively in an automated manner using the fluorogenic stain thioflavin T
(ii) such microclots can aggregate over time, and
(iii) the fibrinaloid microclots may be degraded by nattokinase.
4/5/24 MedRxiV(Sheffield, UK): Increased fibrinaloid microclot counts in platelet-poor plasma are associated with Long COVID https://buff.ly/43Ngdho
Fibrinaloid microclots as a biomarker for Long COVID.
The authors used Thioflavint (ThT) to measure fibrinaloid microclots from platelet-poor plasma and found that there were elevated fibrinaloid microclots in Long COVID and acute COVID infection as compared to controls. In acute COVID infections, the number of fibrinaloid microclots reduced over time.
platelet-poor plasma from Long COVID samples had a higher microclot count compared to control groups but retained a wide distribution of counts. Recent COVID-19 infections were also seen to be associated with microclot counts higher than the control groups and equivalent to the Long COVID cohort, with a subsequent time-dependent reduction of counts.
Figure 2 – Microclot counts from PPP samples.
UC – Uninfected Controls (individuals who have not knowingly been exposed to COVID),
CC – COVID Controls (individuals who have had a positive COVID lateral flow or PCR test in the past),
LC – Long COVID (individuals who self-identify as suffering from persistent symptoms at least three months after a COVID infection).
RC – Recent COVID (individuals who have had a positive COVID lateral flow or PCR test within the previous three weeks).
Figure 3– Microclot counts from PPP samples split by sex. CF – Control female, LCF – Long COVID female, CM – Control male, LCM – Long COVID male.
Work accommodations for Long COVID https://askjan.org/disabilities/Long-COVID.cfm
https://twitter.com/dysclinic/status/1777013493780091010
Long term sequelae of COVID infection in Multiple Sclerosis patients
Multiple Sclerosis patients who got COVID early in the pandemic had similar demographics, but had higher pre-existing major comorbidities. Compared to MS patients without COVID-19, after 3.5 years, MS patients who had COVID-19 had 4x increased mortality risk, 3x increased post infection optic neuritis, >4x need for methylprednisolone treatment for MS relapse and a higher risk of hospitalization (78.92% vs. 66.81%, p<0.01).
4/7/24 Multiple Sclerosis and Related Diseases journal: SARS-CoV-2 infection increases long-term multiple sclerosis disease activity and all-cause mortality in an underserved inner-city population https://buff.ly/4ax5NW2
Retrospective study looked at medical records of 1633 people with Multiple Sclerosis (MS) 3.5 years after COVID infection as compared to MS patients who were not infected with COVID.
MS patients with COVID-19 had similar demographics but higher prevalence of pre-existing major comorbidities
Conclusion: MS patients who survived COVID-19 infection experienced worse long-term outcomes, as measured by treatment for relapse, hospitalization and mortality. Identifying risk factors for worse long-term outcomes may draw clinical attention to the need for careful follow-up of at-risk individuals post-SARS-CoV-2 infection.
Neuro Long COVID
4/8/24 Dani Beckman PhD:
https://twitter.com/DaniBeckman/status/1777248177877573952
“Biomarkers for neuronal damage after Covid infection: even mild or asymptomatic #SARSCoV2 infection leads to reflections of neuron (Nfl marker) and astrocyte (Gfap marker) breakdown in the blood up to 10 months after the resolution of the infection.
“Nfl is a protein only found in neurons. So, if it appears in your blood, you can imagine what it means.
“Now image all these people getting #COVID several times per year.
Protect your neurons, people! Adult neurogenesis in the human brain is not substantial; you are born with all the neurons you have, so you better take good care of them.”
3/18/24 Nature: Neurofilament light chain and glial fibrillary acid protein levels are elevated in post-mild COVID-19 or asymptomatic SARS-CoV-2 cases https://buff.ly/3PWlSMy
Cognitive function and blood tests were performed on 147 people with mild or asymptomatic COVID infection compared to 82 healthy controls (HC) without COVID infection.
Ten months after resolution of mild or even asymptomatic SARS-CoV-2 infection, some people still had abnormal blood levels of NFL and/or GFAP meaning that they had ongoing damage to their brains.
Neurofilament light chain in the serum (sNfL) means that there is ongoing damage to the axons of nerves in the brain (or spinal cord). Glial fibrillary acidic protein (sGFAP) in the blood means that there is abnormal activation of astrocytes in the brain. Astrocytes “perform metabolic, structural, homeostatic, and neuroprotective tasks such as clearing excess neurotransmitters, stabilizing and regulating the blood-brain barrier, and promoting synapse formation” (NIH Stat Pearls) in the brain.
Neurofilament light chain (sNfL) and glial fibrillary acidic protein (sGFAP) in the blood shows that there has been neuron axonal damage and astrocyte activation in the brain and/or spinal cord.
When first assessed, 11 people who had cognitive impairment after asymptomatic or mild COVID infection were found to have significantly higher serum levels of NFL and GFAP. Although these levels decreased over time, the serum levels remained higher than those of the controls who had not had a prior COVID infection. This suggests that after resolution of a mild or asymptomatic COVID infection, there is still ongoing damage to both neurons and astrocytes in the brain and/or spinal cord which may be improving at 10 months, but is still actively ongoing.
"Our results suggest an ongoing damage involving neurons and astrocytes after SARS-Cov2 negativization [resolution], which reduce after ten months even if still evident compared to HCs."
Astrocytes are a subtype of glial cells that make up the majority of cells in the human central nervous system (CNS). They perform metabolic, structural, homeostatic, and neuroprotective tasks such as clearing excess neurotransmitters, stabilizing and regulating the blood-brain barrier, and promoting synapse formation.
From NIH, Stat Pearls
Astrocytes (“star cells”)star-shaped glial cells in the brain and spinal cord. They perform many functions, including biochemical control of endothelial cells that form the blood–brain barrier,[1] provision of nutrients to the nervous tissue, maintenance of extracellular ion balance, regulation of cerebral blood flow, and a role in the repair and scarring process of the brain and spinal cord following infection and traumatic injuries.
From Wikipedia
4/7/24
https://twitter.com/DaniBeckman/status/1777121079104077997
@DaniBeckman PhD: Neuroscientist specialized in high-resolution microscopy at the California National Primate Center.
Biomarkers for #LongCovid
The table below summarizes biomarkers that can potentially indicate differences in long Covid patients and, to some extent, other post-viral illnesses.
All these protein targets can be measured in blood or spinal fluid using commercially available assays, but we know this does not imply patients will have access to them. However, I think it is a good list for patients and M.D.s to discuss together.
I would love to hear from neuro LC patients and neurologists if anyone has experience with measuring GFAP and NFL. Is it two of the proteins I am constantly showing as altered with brain microscopy after the covid infection.
1/20/2023 Frontiers in Medicine, Review: Biomarkers in long COVID-19: A systematic review https://buff.ly/43QrxJH
Long COVID biomarkers: increased IL-6, CRP, TNF-alpha
Neuro Long COVID: high neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP)
Pulm symptoms in LC: high TGF-beta
“the up-regulated levels of neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP) in serum may indicate neuronal damage in the progression of neurodegenerative diseases, such as Alzheimer’s disease (10) or Parkinson’s disease (11).”
Figure 3. Biomarkers significantly associated with different comparison groups. The Venn diagram presents the 13 biomarkers that were reported by two or more eligible studies.
Red indicates up-regulated, while blue refers to down-regulated biomarkers.
Figure 4. Biomarkers of long COVID symptoms. The Venn diagram presents the 41 biomarkers that were reported by two or more eligible studies.
Red indicates up-regulated, while blue refers to down-regulated biomarkers.
Supplementary: PubMed search terms used for this article https://www.frontiersin.org/articles/10.3389/fmed.2023.1085988/full#supplementary-material
ME/CFS Severity Score by Whitney Dafoe
4/7/24 Frontiers Immunology: Longitudinal cytokine and multi-modal health data of an extremely severe ME/CFS patient with hypermobility spectrum disorder (HSD) reveals insights into immunopathology, and disease severity https://buff.ly/3TXhJt7
Whitney Dafoe, Ron Davis
Updated ME/CFS Severity Scale
" Our study advocates for the integration of longitudinal multi-omics with multi-modal health data and artificial intelligence (AI) techniques to better understand ME/CFS and its major comorbidities. These findings highlight the significance of dysregulated Th2-type cytokines in patient stratification and precision medicine strategies. Additionally, our results suggest exploring the use of low-dose drugs with partial agonist activity as a potential avenue for ME/CFS treatment."
TH1 and TH2 are two types of T cells called T helper cells. Th1 cells send out cytokines including Interferon gamma (IFNγ) to recruit macrophages to destroy infected cells or cancer cells. Th2 cells make Interleukin-13 (IL-13), a cytokine that helps to activate B cells to make antibodies to neutralize pathogens like viruses and bacteria.
4/9/24 KFF: As Recommendations for Isolation End, How Common is Long COVID? https://buff.ly/4cR9Rlr
In March 2024, the CDC changed isolation recommendations for COVID to be more like the flu.
Among the 60% of U.S. adults who have had COVID, roughly 3 in 10 report having long COVID at some point and roughly 1 in 10 report having long COVID now (Figure 1).
An estimated 17 million adults currently have long COVID.
Among adults with long COVID, 79% report having any activity limitations from long COVID and 25% report that long COVID limits their activities “a lot” (Figure 2).
Looking ahead, 5% to 10% of adults in the U.S. may continue to experience long COVID at any point in time, but research to improve diagnosis and treatment moves slowly.
AI:
4/8/24 National Academy of Medicine: Artificial Intelligence in Health, Health Care, and Biomedical Science: An AI Code of Conduct Principles and Commitments Discussion Draft https://buff.ly/49EegWc
Other news:
4/11/24 Rare genetic variation in fibronectin 1 (FN1) protects against APOEε4 in Alzheimer’s disease - Acta Neuropathologica https://buff.ly/3vVUasn
Eric Topol: People with 2 copies of APOE4 have ~10X risk of Alzheimer's. Here's the discovery of a protective variant and learning how fibronectin 1 plays a role
4/5/24 Washington Post: An Ozempic baby boom? Some GLP-1 users report unexpected pregnancies. https://buff.ly/3PY6MpU
The fat cells in our bodies make estrogens. Decreasing body fat can cause some women, such as women with PCOS, to ovulate. Alternatively, it is unknown if birth control pills are as effective with GLP-1 medications.
4/8/24 Nature Human Behaviour: A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions https://buff.ly/43T9aE4
The Irony
4/8/24 Total Solar Eclipse
https://flowingdata.com/2024/04/08/airbnb-occupancy-along-the-eclipse-path/
https://twitter.com/Aiims1742/status/1776759027483238894
Anirban Maitra got this welcome kit from his Airbnb host:
Eclipse gum, Starry soda, Sun chips and Moon Pies, as well as eclipse glasses




















































Everyday I read about covid related items but I always find something new on your substack that I have not read. And even the journal articles that I have read, your summaries always bring to my attention something I missed. Thanks so much.
Thank you. ❤️