COVID news 2/18/23
Hi all,
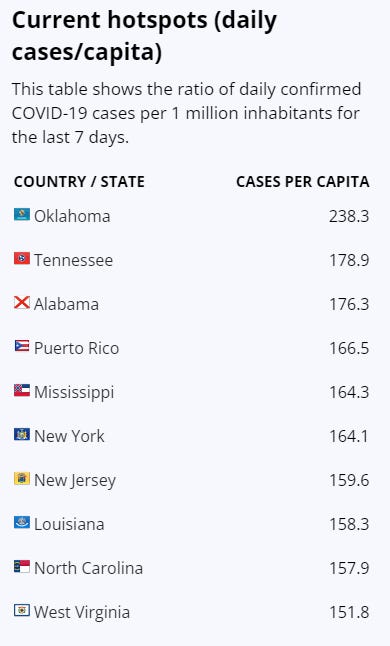
This week, XBB.1.5 is up to 80% of COVID infections in the US. There are still no other variants putting pressure on XBB.1.5 yet which is reassuring. Hospitalizations have decreased as have deaths. We are in a better place than over the winter holidays. Here in the Bay Area, wastewater in San Mateo county, San Francisco, Oakland and Napa shows an increase of virus in wastewater, so we may see an increase in cases in the next 1-2 weeks per Dr. Bob Wachter.
Masks
A recent Cochrane review stated that “there is uncertainty about the effects of face masks”. However, Dr. Linsey Marr, an expert on airborne virus transmission and mask technology, said that there were limitations with the Cochrane review that included many studies that were conducted during non-epidemic influenza periods with lower respiratory viral circulation and transmission compared to COVID-19. Also, many of the studies included in the review were of healthcare workers who wore masks at work but not at home or while interacting with people in their community. She pointed to the recent CDC study showing that N95 masks reduced COVID by 83%, surgical masks by 66% and cloth masks by 56% if they were worn in indoor public settings.
Neuro Long COVID and the Brain
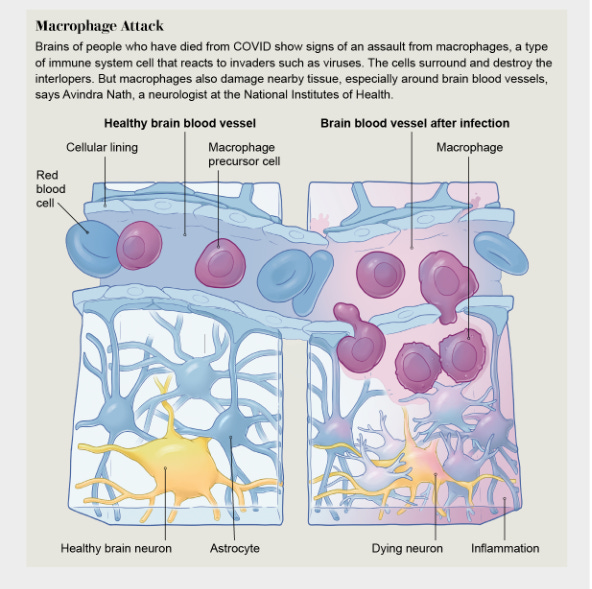
There were several excellent articles on Long COVID and the brain this week. First, Dr. Wes Ely presented 2 people with Long COVID who told their stories of “brain fog”, problems in executive function, memory, and processing speed, and difficulty finding words after a COVID infection. He reviewed more than 20 articles on neuropathology after COVID, and discussed possible causes of inflammation in the brains of long COVID patients including glial cell activation in brain white matter which can harm gray matter neurons in the brain, loss of brain tissue in some, and impaired metabolism in the brains of other people with Long COVID. A preprint in the Lancet looking at Mendelian randomization showed that COVID infection can cause atrophy in specific brain regions. Severe initial COVID infections were found to cause more extensive brain atrophy.
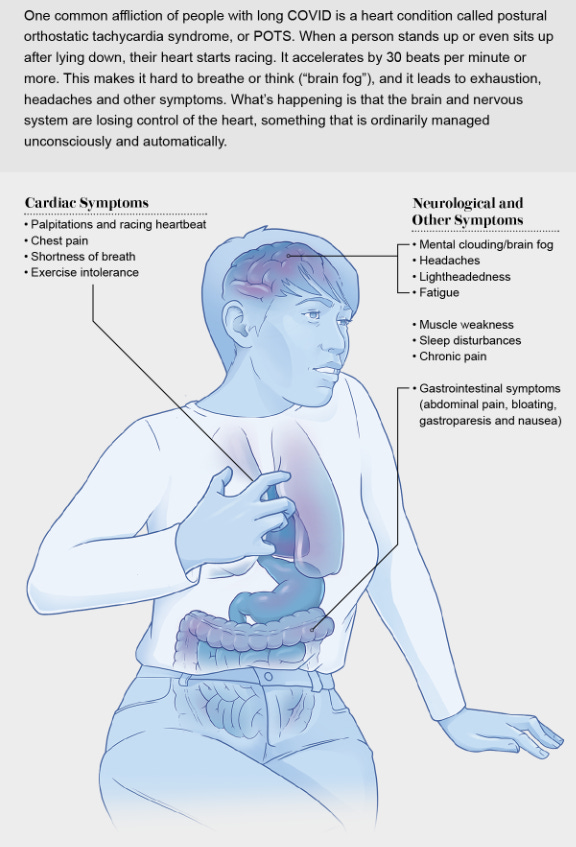
Finally, Scientific American had an article with great graphics entitled “Long COVID Now Looks like a Neurological Disease, Helping Doctors to Focus Treatments” discussing dysfunction of the autonomic nervous system, postural orthostatic tachycardia syndrome (POTS), cognitive dysfunction, also known as “brain fog”, and other neurologic symptoms of Long COVID. The autonomic nervous system travels is responsible for unconscious functions such as the regulation of the heart beating, breathing, sweating and blood vessel dilation. Dysfunction of the autonomic nervous system can cause POTS resulting in a racing heart beat with sitting or especially with standing, fatigue and even bowel or bladder issues. Additionally, POTS may be associated with post-exertional malaise (PEM), or exhaustion after routine activities such as walking, thinking or talking on the phone. Post-exertional malaise is also a feature of ME/CFS.
Long COVID
Dr. Iwasaki and Dr. Putrino published an Op-Ed in the Lancet yesterday about suspected triggers for Long COVID- viral persistence, autoantibodies, reactivation of latent viruses like EBV and immune dysregulation. They discussed the importance of well thought out clinical trials and the inclusion of people with other post-infectious disease syndromes like ME/CFS and Lyme’s Disease. A meta-analysis in the Lancet looked at 65 studies on Long COVID which showed that prior COVID infections, even with Omicron, can provide fairly long lasting protection against severe disease in the case of a COVID reinfection. But, with reinfections comes the increased risk of Long COVID.
A fascinating and somewhat scary article came out yesterday from Charite Berlin showing that in Long COVID patients with post-exertional malaise (PEM), their muscles show abnormal microvasculature including fewer capillaries, increased macrophages in muscle tissue and gene signatures showing immune dysregulation and altered metabolic pathways. The authors theorize that the initial COVID infection may cause immune-mediated structural changes of the microvasculature in skeletal muscles, potentially explaining the exercise-dependent fatigue and muscle pain.
A new study from UCSF shows that people with Long COVID have problems with their immune systems with increased CD4 T cells, exhausted SARS-CoV-2-specific CD8 T cells, and higher levels of SARS-CoV-2 antibodies. B cells which make antibodies and the T cells which help attack foreign invaders usually “talk” with each other via chemical messages to provide a coordinated immune response. But, in people with Long COVID, this study showed that there is no longer “proper crosstalk between the humoral (B cell) and cellular (T cell) arms of adaptive immunity.”
A meta-analysis this week shows that vaccination before a COVID infection can reduce the risk of Long COVID by 36%. But, getting a vaccination after someone has Long COVID, helps reduce symptoms by only 20%. A study in the Royal Society of Medicine Journal showed in a prospective study of people with Long COVID that one year after acute COVID infection, organ impairment such as extreme breathlessness or brain fog continued in 59% of people. In people that were hospitalized in China with the original strain of SARS-CoV-2 in early 2020 and had abnormal lung CT scans at the time that they were discharged from the hospital, one third of patients had persistent interstitial lung abnormalities (ILAs) on lung CT scan and had continued respiratory symptoms 2 years later. The Columbia University surgery department reports that 1 in 10 lung transplants performed are in people whose lungs were damaged by COVID.
Diabetes
Many studies have shown that getting a COVID infection can increase your risk of new onset diabetes. A new article from Cedar Sinai shows that COVID infections, including infections from the Omicron variant, increase a person’s risk for diabetes by 58% in the 90 days after infection. This study also showed that COVID vaccination decreased the risk of diabetes.
Paxlovid and antivirals
Regarding viral rebound, scientists in Hong Kong report that Paxlovid was not associated with an increase in rebound in hospitalized patients. When it did happen, viral rebound was more common in immunocompromised people, those with more medical comorbidities and in patients taking corticosteroids. Viral rebound was not associated with adverse clinical outcomes however. During the Omicron wave in Ontario, Canada and the BA.4/5 Omicron wave in Colorado, Paxlovid significantly decreased hospitalizations and deaths, independent of vaccination status, age, or variant.
Other news, my SMFM
Finally, there were several interesting articles from the Society of Maternal and Fetal Medicine meeting showing that early cannabis use in pregnancy being associated with adverse outcomes and that people with hypertension in pregnancy have increased risks of cerebrovascular disease, cardiomyopathy, heart failure, and chronic hypertension in the 2 years after pregnancy. In pregnant people with chronic hypertension and diabetes, keeping their blood pressure below 130/80 mm Hg was associated with a 57% lower risk of a composite of adverse clinical events.
Stanford researchers used a deep learning model to predict outcomes in a newborn baby’s health using EHR medical record data from the mother. A Nature article this week, discusses “how a pioneering diabetes drug offers hope for preventing autoimmune disorders.” Teplizumab may help delay a Type I Diabetes diagnosis in people at high risk and giving oral insulin powder to children may help prevent future autoimmune attacks on the pancreas via regulatory T cells. And finally, I have included a review of hallmarks or neurodegenerative diseases that may help define pathogenic mechanisms to help design personalized therapies for neurodegenerative diseases such as Parkinson’s disease, ALS and others.
Have a good weekend,
Ruth Ann Crystal MD
Twitter: https://twitter.com/CatchTheBaby
COVID news:
World: https://medriva.com/charts/world-monitor.php
USA: https://medriva.com/charts/usa-monitor.php
https://www.nytimes.com/interactive/2021/us/covid-cases.html
US cases:
US hospitalizations:
Walgreens positivity rate: https://www.walgreens.com/businesssolutions/covid-19-index.jsp
Variant tracker in US: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
XBB.1.5 is 80% and no other variants are showing gains.
Wastewater Monitoring:
CDC Wastewater Monitor https://covid.cdc.gov/covid-data-tracker/#wastewater-surveillance
Biobot: https://biobot.io/data/
Wastewater in LA county (since 2020 and over last 6 months)
Sewer Coronavirus Alert Network (SCAN) project by Stanford University:
San Mateo county
2/17/23
2/16/23 Healio: Q&A: What a major review does and does not tell us about masks and COVID-19 https://buff.ly/3k97JPw
Regarding the newly reported Cochrane Database Review on masks, many studies were conducted during non-epidemic influenza periods” and “in the context of lower respiratory viral circulation and transmission compared to COVID-19.”
2/11/23 CDC: Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California https://buff.ly/3Lbo2UI
2/14/23 Lancet ID Op Ed (Akiko Iwasaki and David Putrino): Why we need a deeper understanding of the pathophysiology of long COVID https://buff.ly/3I78GQf
Long COVID or post-acute sequelae SARS-CoV-2 infection (PASC) has several subtypes.
The main disease hypotheses for the root causes of long COVID include
viral persistence (infectious virus, viral RNA, or viral proteins),
autoimmunity triggered by the infection,
reactivation of latent viruses, and
inflammation-triggered chronic changes leading to tissue dysfunction and damage.
Molecular, cellular, and physiological analyses are needed to understand the root causes of each long COVID endotype.
Possible treatments:
Persistent viral infection could be targeted by antivirals;
Long COVID driven by autoimmune disease could be treated using monoclonal antibodies that target lymphocytes or drugs that block cytokines and cytokine signaling
Reactivation of herpesviruses contributes to disease, targeting such viruses using antivirals or vaccines could be considered.
Diagnostic criteria considering the root causes to prevent and treat long COVID will require large longitudinal studies.
Inclusion of individuals with other forms of post-acute infection syndrome (PAIS) such as ME/CFS and Lyme’s disease as comparison groups in long COVID research is important for broadening overall understanding and widening the impact of this research.
2/16/23 Lancet: Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis https://buff.ly/3YEFF5B
Meta-analysis of 65 studies
Having a prior infection with ancestral, alpha, delta, and beta variants protected well (85%) against reinfection, any symptomatic disease, and severe disease with reinfections.
However, protection from a prior Omicron infection was a lot less (only 55%) against reinfection and protection waned rapidly over time.
Prior Omicron infection did help protect against severe disease, but not much data.
But, reinfection is a major risk for Long COVID.
Long COVID and the Brain
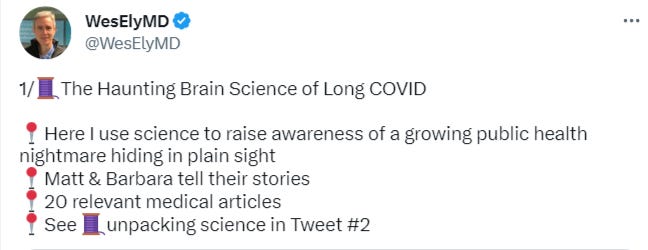
2/16/23 @WesElyMD
2/16/23 Wes Ely MD in STAT news: The haunting brain science of long Covid https://buff.ly/3IuL4X2
More than 65 million people around the world have Long COVID.
SARS-CoV-2 virus can persist in the body.
2 people with Long COVID tell their stories of “brain fog”, problems in executive function, memory, and processing speed, and difficulty finding words.
Many people with Long COVID have post exertional malaise (PEM) which is a condition characteristic of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) where even slight exertion leaves people inexplicably incapacitated for hours or days.
Review of possible causes of brain inflammation including activated glial cells in brain white matter that can affect gray matter neurons in the brain, loss of brain tissue in some, and impaired metabolism in the brains of some people with Long COVID.
Twitter thread by Dr. Wes Ely reviewing more than 20 studies on neuropathology seen in people with Long COVID.
2/16/23 Lancet Pre-print: Causal Effects of COVID-19 on Structural Changes in Specific Brain Regions: A Mendelian Randomization Study https://buff.ly/3lJILq5
Mendelian randomization shows that COVID infection can cause atrophy in specific brain regions.
Severe initial COVID infections show more extensive brain atrophy.
2/14/23 Sci Am: Long COVID Now Looks like a Neurological Disease, Helping Doctors to Focus Treatments https://buff.ly/3Sii88h
Comprehensive article reviewing autonomic dysfunction, POTS, brain fog and other neurologic symptoms of Long COVID.
“As of February 2022, the syndrome [Long COVID] was estimated to affect about 16 million adults in the U.S. and had forced between two million and four million Americans out of the workforce, many of whom have yet to return. Long COVID often arises in otherwise healthy young people, and it can follow even a mild initial infection.”
The autonomic nervous system goes from the brain or spinal cord to the entire body. It is responsible for unconscious functions such as heartbeat, breathing, sweating and blood vessel dilation.
Dysfunction of the autonomic nervous system is called Dysautonomia.
For many people with long COVID, dysautonomia takes the form of postural orthostatic tachycardia syndrome, or POTS.
POTS causes a racing heart beat with sitting or especially with standing, fatigue and it can cause bowel or bladder issues.
POTS may also be a part of post-exertional malaise (PEM), or exhaustion after thinking, talking, walking or other regular activities. Post-exertional malaise is a feature of ME/CFS (
Treatments for POTS include beta blockers to decrease the heart rate and ivabradine.
Adderall, usually used for ADHD, can help with brain fog.
Even after starting medication which can help patients feel better, they can have flare-ups of debilitating symptoms.
POTS (Postural Orthostatic Tachycardia Syndrome)
2/16/23 MedRxiV (Charite Berlin): Post-COVID syndrome (PASC, Long COVID) is associated with capillary alterations, macrophage infiltration and distinct transcriptomic signatures in skeletal muscles https://buff.ly/3SliOd3
Muscle biopsies obtained from 11 patients suffering from severe fatigue and post-exertional malaise (PEM) after an infection with SARS-CoV-2.
Compared to two independent historical control cohorts.
Muscle biopsies from Long COVID patients with PEM had:
Microvascular abnormalities (thicker capillary basement membranes)
Fewer capillaries
Increased CD169+ macrophages
No SARS-CoV-2 RNA was found in the muscle
Distinct gene signatures with immune dysregulation and altered metabolic pathways.
Hypothesis: The initial viral infection may have caused immune-mediated structural changes of the microvasculature, potentially explaining the exercise-dependent fatigue and muscle pain.
Fig. 2. Type-2b-fiber atrophy and increased numbers of tissue macrophages in skeletal muscles of patients with PCS
Fig. 3. Decreased capillary-to-fiber ratio and thicker capillary basement membranes in patients with PCS
2/11/23 BioRxiV (UCSF): Long COVID manifests with T cell dysregulation, inflammation, and an uncoordinated adaptive immune response to SARS-CoV-2 https://buff.ly/3IrQ52V
People with Long COVID (LC) had
Increased CD4+ T cells and exhausted SARS-CoV-2-specific CD8+ T cells.
Higher levels of SARS-CoV-2 antibodies.
SARS-CoV-2-specific T cell and B cell (antibody) responses are uncoordinated.
“Collectively, our data suggest that proper crosstalk between the humoral and cellular arms of adaptive immunity has broken down in LC, and that this, perhaps in the context of persistent virus, leads to the immune dysregulation, inflammation, and clinical symptoms associated with this debilitating condition.”
2/8/23 Vaccine: Protective effect of COVID-19 vaccination against long COVID syndrome: A systematic review and meta-analysis https://buff.ly/3jUegxo
One or two dose initial vaccination reviewed from 6 studies. Boosters not included.
36% lower risk of long COVID for vaccination before SARS-CoV-2 infection.
Among those with ongoing long COVID:
54% did not report symptomatic changes after vaccination
20% did report symptomatic improvement two weeks to six months after vaccination.
2/15/23 The Atlantic: What Not to Ask Me About My Long COVID https://t.co/e7rgrepONp
In a thread discussing her article, Jennifer Senior says:
Don’t ask me if I am getting better.
Symptoms can change.
It’s depressing.
Be gentle with us. Don’t judge; don’t pity.
2/14/23 Royal Society of Medicine Journal: Multi-organ impairment and long COVID: a 1-year prospective, longitudinal cohort study https://buff.ly/3YxsdR1
PASC, Long COVID prospective study
At 6 months and 12 months after COVID infection:
Extreme breathlessness (38% at 6 months and 30% at 12 months),
Cognitive dysfunction (48% and 38%)
Poor health-related quality of life (57% and 45%)
Symptoms were associated with female gender, younger age and single-organ impairment.
Organ impairment persisted in 59% of 331 individuals followed up at 1 year post COVID-19, with implications for symptoms, quality of life and longer-term health, signaling the need for prevention and integrated care of long COVID.
2/14/23 Radiology: Longitudinal Assessment of Chest CT Findings and Pulmonary Function in Patients after COVID-19 https://buff.ly/3IvgQ6n
PASC, Long COVID prospective study
144 patients discharged from the hospital after SARS-CoV-2 infection between January 15 and March 10, 2020 were followed with CT scans at 6 months, 12 months, 2 years.
Pre Vaccination in 2020. The study only included people with abnormal CT lung on discharge from hospital.
More than one third of participants had persistent interstitial lung abnormalities (ILAs) at 2 years, which were associated with respiratory symptoms and decreased diffusion pulmonary function.
Participants with fibrotic ILAs more commonly suffered from respiratory symptoms (45% vs 17%, P = .03) and had a lower diffusing capacity of the lung for carbon monoxide (60% vs 22%, P = .005) than those with non-fibrotic ILAs.
2/11/23 One in Ten Lung Transplants Go to Covid-19 Patients: Here’s What We Know | Columbia Surgery https://buff.ly/3DZ0MXS
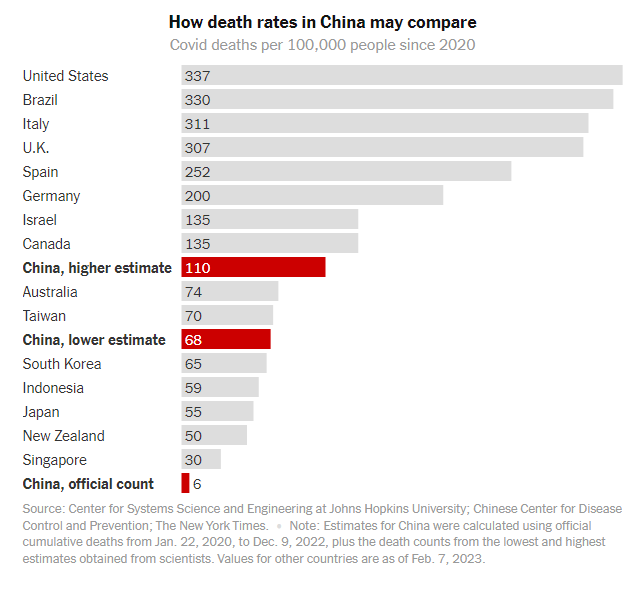
2/15/23 NY Times: How Deadly Was China’s Covid Wave? https://buff.ly/3xyNCxk
Two months after China ended “zero Covid,” rough estimates suggest that between 1 and 1.5 million people died — far more than the official count.
Compared to other countries
Diabetes:
2/14/23 JAMA (Cedars Sinai): COVID-19 Vaccination and Risk for Incident Diabetes After COVID-19 Infection https://buff.ly/3IqvrQH
Cohort study showed that COVID infection was associated with increased risk of diabetes (adjusted odds ratio 1.58) seen with Omicron infection and infections prior to Omicron.
Vaccinated people had a lower risk of diabetes, suggesting a benefit of vaccination.
Increased risk of new onset diabetes after COVID infection seen in many prior studies:
3/21/22 Risks & burdens of incident diabetes in long COVID:cohort study https://buff.ly/3qqe5Ka
3/2022 Incidence of newly diagnosed diabetes after Covid-19 https://buff.ly/3qbnh4Q
5/2022 Rising diabetes diagnosis in long COVID https://buff.ly/3JMvAw5
5/2022 Post-acute sequelae of COVID-19: A metabolic perspective https://buff.ly/3iJM4cj
11/2022 Association of COVID-19 with diabetes: a systematic review and meta-analysis
In the lay press:
COVID-19 tied to greater risk of diabetes, but COVID-19 vaccination diminishes risk
CNN (2/14, Goodman) reports people who have had COVID-19 “have a higher risk of developing diabetes, and that link seems to have persisted into the Omicron era, a new study” published in JAMA Network Open found. The researchers found COVID-19 “increased the odds of a new diabetes diagnosis by an average of about 58%.”
Paxlovid and Antivirals
2/13/23 Lancet ID: Viral burden rebound in hospitalised patients with COVID-19 receiving oral antivirals in Hong Kong: a population-wide retrospective cohort study https://buff.ly/3lzKIFL
Viral burden rebound rates are similar between patients with antiviral treatment (Paxlovid or Molnupiravir) and those without.
Importantly, viral rebound was not associated with adverse clinical outcomes.
During the omicron BA.2.2 wave, viral burden rebound did not differ significantly in:
6·6% receiving Paxlovid (nirmatrelvir–ritonavir),
4·8% receiving molnupiravir,
4·5% in the control group.
Immunocompromised people had increased odds of viral burden rebound, regardless of antiviral treatment:
Among patients receiving Paxlovid (nirmatrelvir–ritonavir), the odds of viral burden rebound were higher in:
those aged 18–65 years (vs >65 years; 3·09, p=0·050),
those with high comorbidity burden (score >6 on the Charlson Comorbidity Index; 6·02 [2·09–17·38], p=0·0009),
those concomitantly taking corticosteroids (7·51 [1·67–33·82], p=0·0086);
2/13/23 Lancet Editorial:SARS-CoV-2 rebound with and without antivirals https://buff.ly/3jZdleX
"Given that no association was found between oral antiviral treatment and viral burden rebound ... emphasizes the importance of continuing to offer antivirals to individuals with COVID-19 who are at increased risk of progression."
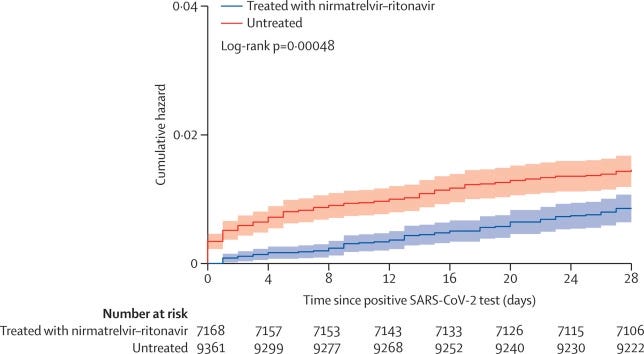
2/13/23 CMAJ (Ontario): Population-based evaluation of the effectiveness of nirmatrelvir–ritonavir (Paxlovid) for reducing hospital admissions and mortality from COVID-19 https://buff.ly/3YV2MIU
Paxlovid (nirmatrelvir–ritonavir) given during Omicron:
44% reduction in hospitalizations
51% reduction in deaths (more in age 70+)
Findings were similar across strata of age, drug–drug interactions, vaccination status and comorbidities.
2/10/23 Lancet: Real-world use of nirmatrelvir–ritonavir (Paxlovid) in outpatients with COVID-19 during the era of Omicron variants including BA.4 and BA.5 in Colorado, USA: a retrospective cohort study https://buff.ly/40Sq6c0
In a real-world study, Paxlovid decreased hospitalizations by 55% and deaths by 85%, independent of vaccination status, age, or variant.
2/10/23 Lancet: Long-term effectiveness of COVID-19 vaccines against infections, hospitalisations, and mortality in adults: findings from a rapid living systematic evidence synthesis and meta-analysis up to December, 2022 https://buff.ly/3xhKDsR
A review of 68 vaccine effectiveness studies.
Vaccine effectiveness (VE) decreases over time against COVID infection, but protection against hospitalizations and death is preserved for about 6 months.
For any SARS-CoV-2 infection:
VE for the primary series reduced from 83% at baseline (14–42 days) to 62% by 112–139 days.
VE at baseline was 92% for hospitalisations and 91% for mortality, and reduced to 79% at 224–251 days for hospitalisations and 86% at 168–195 days for mortality.
For Omicron:
variant for infections, hospitalisations, and mortality at baseline compared with that of other variants, but subsequent reductions occurred at a similar rate across variants.
For booster doses (mostly Omicron variant):
For infection, 70% VE at baseline went to 43% by 112 days.
For hospitalizations, 89% VE at baseline down to 71% protection 112 days later.
2/7/23 Nature: COVID drug drives viral mutations — and now some want to halt its use https://buff.ly/3JXOh2K
Molnupiravir does not improve hospitalizations or death rates from COVID, but it does cause mutations in the virus which could be dangerous. It should be removed from the market.
Other news:
2/9/23 AJOG: Early pregnancy cannabis exposure and adverse pregnancy outcomes https://buff.ly/3RTUfmY
For more than 9,000 pregnancies, small for gestational age, medically indicated preterm birth, stillbirth, or hypertensive disorders of pregnancy occurred in 27.4% of the cannabis-exposed group compared with 18.1% of the non-exposed group.
2/11/23 MedPage Today: Women With Hypertension During Pregnancy (HDP) Face Higher CVD Risks https://buff.ly/3HWSLUH
Within 2 years postpartum, patients with HDP had almost 2x the risk for cerebrovascular disease, nearly 3x the risk for cardiomyopathy and heart failure (HF), and 7x the risk for chronic hypertension (HTN).
2/13/23 MedPage Today: Lower Blood Pressure Better in Pregnancy With Diabetes https://buff.ly/3k5CJQj
Presentation by Lorie M. Harper, MD, MSCI at SMFM.
"In a secondary analysis of the CHAP study, a blood pressure below 130/80 mm Hg was associated with a relative 57% lower risk of a composite of adverse clinical events" pregnant people with chronic hypertension and diabetes:
22.6% complications for blood pressure below 130/80 mm Hg
51.6% complications for blood pressures in the 130-139/80-89 mm Hg range
Comparing the lower and higher blood pressure groups:
Preeclampsia with severe features occurred in 19.4% vs 43.8% (P<0.01)
Indicated preterm birth before 35 weeks of gestation occurred in 8.3% vs 23% (P<0.01)
Placental abruption occurred in two vs six cases (less than 1% vs 2.8%, P=0.50)
“The CHAP study was originally designed to confirm the safety and benefit in pregnancy of the otherwise standard recommendation for reducing blood pressure to under 140/90 mm Hg compared to withholding blood pressure medication until women reached severe hypertension (>160/105 mm Hg). It changed the field by showing that lower was better, without harming babies or mothers.”
2/15/23 Science (Stanford): Data-driven longitudinal characterization of neonatal health and morbidity https://buff.ly/3xpIBqN
"Using two cohorts with a total of 27,000 mothers linked to more than 32,000 neonates and validated externally with more than 12,000 newborns, we demonstrated the ability to serially and comprehensively predict neonatal outcomes from various maternal conditions extracted from EHRs."
2/15/23 Nature: How a pioneering diabetes drug offers hope for preventing autoimmune disorders https://buff.ly/3YY1FrW
Teplizumab is an antibody that blocks T cells to stop them from destroying insulin-producing islet cells in the pancreas. Given to people before Type I Diabetes (T1D) diagnosis, who have two or more autoantibodies against islet cells and signs of altered sugar metabolism.
Oral insulin powder eaten by children daily caused them to develop a special type of immune cell, known as a regulatory T cell, that helps protect against future autoimmune attacks.
Regarding another autoimmune disease, Multiple Sclerosis (MS), dimethyl fumarate given to people with a distinct type of anomalous brain scan helps reduce the risk of MS by more than 80% compared with a placebo.
2/16/23 Cell: Hallmarks of neurodegenerative diseases https://buff.ly/3YDY8ir